Amy Carpenter Aquino
May 2023—How to distinguish appendiceal diverticular disease and appendiceal polyps from mucinous neoplasms was just part of a CAP22 course on appendiceal lesions, led by Maryam Pezhouh, MD, MSc, of the University of California, San Diego, and Jacqueline Birkness-Gartman, MD, of Johns Hopkins University School of Medicine.
Their cases and comments covered mimics and more as they took attendees through inflammatory lesions, structural abnormalities, polyps, and gynecologic proliferations that involve the appendix. (Their comments on neoplasms and adenocarcinomas will be published separately.)
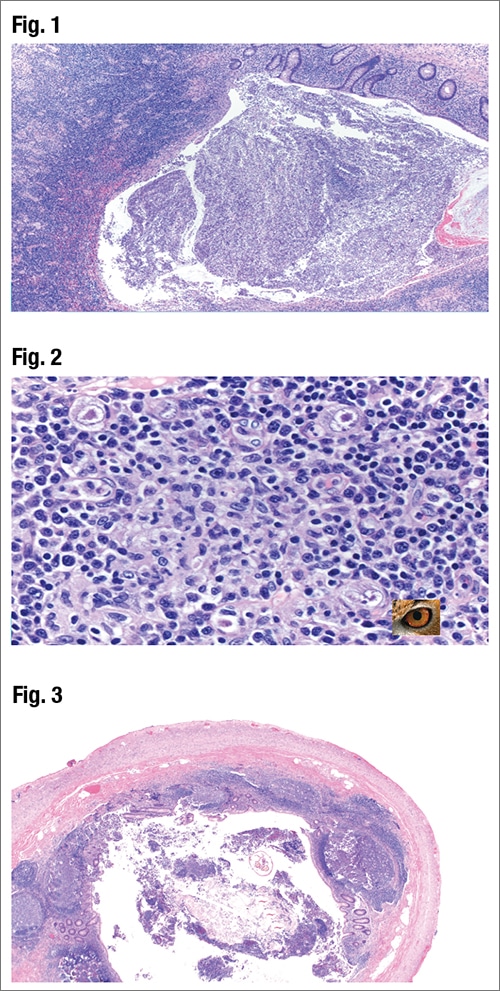
In her talk on inflammatory lesions of the appendix, Dr. Pezhouh, associate professor of pathology, reported on the case of a 45-year-old female who presented to the emergency room with abdominal pain, vomiting, and nausea. The patient’s medical history included a renal transplant. Imaging was consistent with acute appendicitis and the patient underwent an appendectomy. Fig. 1 reveals “the mucosa is basically ulcerated” with a lot of acute and chronic inflammation, Dr. Pezhouh said. In Fig. 2 large cells with characteristic cytomegalovirus (CMV) nuclear inclusions also known as “owl eye” are seen. Immunostain (not shown) highlighted the infected cells.
“In acute appendicitis, we usually don’t look for CMV,” Dr. Pezhouh said, but it should be considered in patients with a history of solid organ transplant or HIV or who are very young or very old.
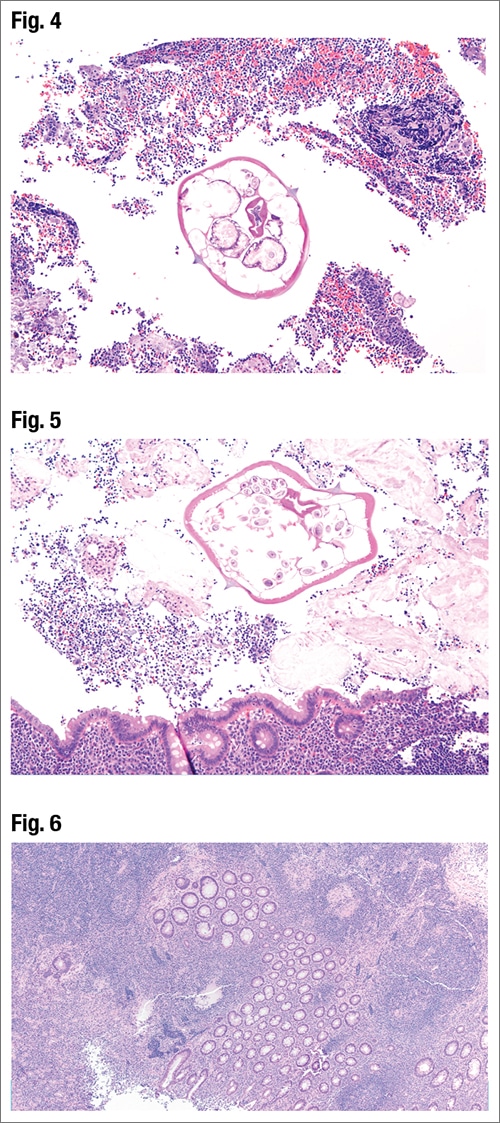
In the case of an eight-year-old boy who presented with abdominal pain and signs of acute appendicitis and who underwent an appendectomy, Dr. Pezhouh said inflammatory cells were seen in the lumen of the appendix and, on higher power, something else could also be seen in the lumen (Fig. 3). In Fig. 4 is a cross-section of a worm in the lumen, and in Fig. 5 is another worm or another section of the same worm, and eggs can be seen. It is Enterobius vermicularis, or pinworm, for which lateral alaes are characteristic. Furthermore, typically Enterobius vermicularis eggs are plano-convex with one flattened side and one convex side. Enterobius vermicularis usually affects children ages seven to 11 and is an incidental finding, she said. Sometimes a mass of worms can cause obstruction in the GI tract or appendix, and occasionally pinworm can be associated with acute appendicitis. “Adult worms can also migrate to the lower genital tract and cause a granulomatous reaction, and the same goes for the appendix,” Dr. Pezhouh said, though there were no granulomas in the case she reported.
In cases of a perforated appendix, sometimes clinicians treat the patient with antibiotics, discharge the patient, and perform an appendectomy later, as in the case of a 28-year-old male who presented with typical signs and symptoms of acute appendicitis and had surgery four weeks later, Dr. Pezhouh said. Sections of the appendix were inflamed, with a lot of lymphoid follicles and some focal acute inflammation, she said, but mostly chronic inflammation. Fairly well-formed granulomas are also seen in Figs. 6 and 7.
“When you see granulomas in the appendix, you know the differential is long,” she said, one of which is interval (or delayed) appendicitis (when the patient has a ruptured appendix, is treated with antibiotics, and has an appendectomy four to eight weeks later). Its histologic features are variable and may include residual focal acute inflammation. Often seen is transmural chronic inflammation with lymphoid aggregates. Granulomatous inflammation is common (about 60 percent of the time). “You may see fibrosis often in the area that was perforated,” post-healing, she said, and xanthogranulomatous appendicitis can be seen in a subset of cases.
Granulomatous appendicitis is a rare diagnosis, she said—around 0.1 to two percent of appendectomies can have granulomas. “It usually resembles acute appendicitis” and usually doesn’t recur. “Only five to 10 percent of the patients can develop Crohn’s disease in the GI tract,” she said. It is usually idiopathic but can be caused by Yersinia, Myobacterium tuberculosis, Enterobius vermicularis, a foreign body, interval appendicitis, and sarcoidosis, among other causes. “So remember the mimics and other etiologies to be considered before labeling the patient with Crohn’s disease whenever you see granulomas,” Dr. Pezhouh said.
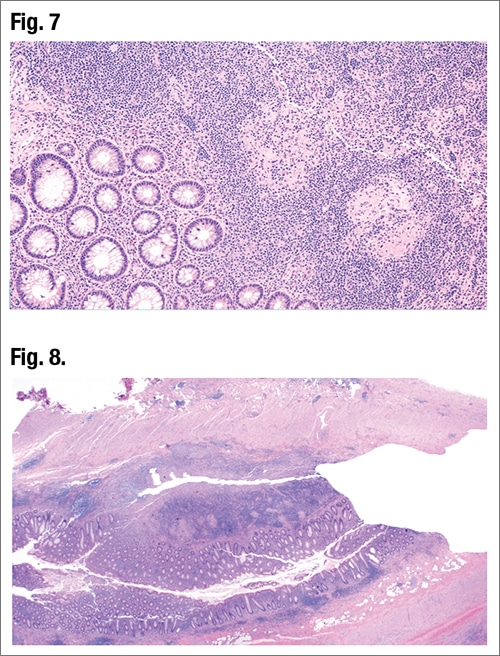
In Fig. 8 is an example of Crohn’s disease as seen in a longitudinal section of the appendix. It was the case of a 36-year-old female with a past medical history of Crohn’s disease and refractory treatment who presented for ileocolonic resection, Dr. Pezhouh said. The inflammation is transmural. In Fig. 9 granulomas are visible with focal areas of mild acute inflammation.
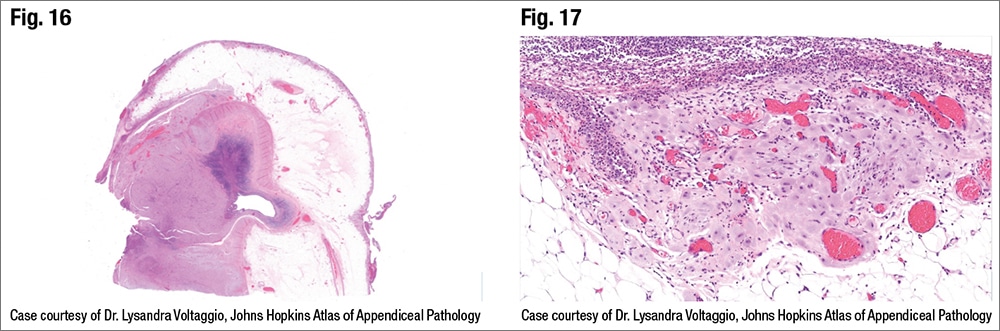
Gynecologic proliferations involving the appendix can take the form of endometriosis, endosalpingiosis, and decidual lesions, said Dr. Birkness-Gartman, assistant professor of pathology at Johns Hopkins. Endometriosis consists of endometrial-type glands and often has associated endometrial stroma, and there can be hemorrhage and hemosiderin-laden macrophages, she said. Endosalpingiosis consists of glands or cystic structures lined by tubal-type epithelium without associated stroma. “And decidual lesions can consist of decidualized endometriosis where you have decidualized stroma with some retained glands,” she said, “or deciduosis where you do not have glands.”
Dr. Birkness-Gartman presented the case of a 40-year-old woman with known endometriosis who underwent a diagnostic laparoscopy, which revealed endometriosis involving both ovaries, the appendix, and the colonic serosa. The patient underwent a hysterectomy with bilateral salpingo-oophorectomy and appendectomy. In Fig. 10 is a fibrotic-appearing lesion involving the appendix (arrows). In Fig. 11 are glands that appear to be infiltrating the muscularis propria.
In Fig. 12 is “the typical histology of endometriosis,” she said, noting the endometrial-type glands, “and one of the clues to the diagnosis is the spindled endometrial-type stroma surrounding the glands.”
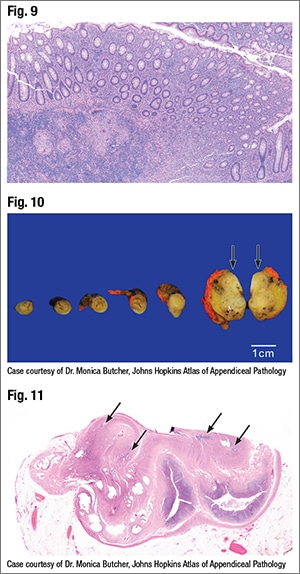
Noor, et al., reported finding in a review of cases that appendiceal endometriosis affects women with a median age of 34, Dr. Birkness-Gartman said, “and this could present with acute appendicitis, intussusception, or GI bleeding” (Noor M, et al. Hum Pathol. 2019;92:101–106). They found that 73 percent of patients with appendiceal endometriosis had extra-appendiceal involvement, “but interestingly,” she said, “those who presented with acute appendicitis were less likely to have extra-appendiceal involvement” (22 percent). Histologically, appendiceal endometriosis typically involves the muscularis propria but can involve the serosa, she said. Glands can have an infiltrative-appearing growth pattern, “which could raise concern for adenocarcinoma.” However, endometrial-type stroma, hemorrhage, and hemosiderin-laden macrophages are clues to the correct diagnosis, she said. IHC can be helpful because endometrial-type glands will label for CK7 and ER, and the stroma will label for CD10 and ER.
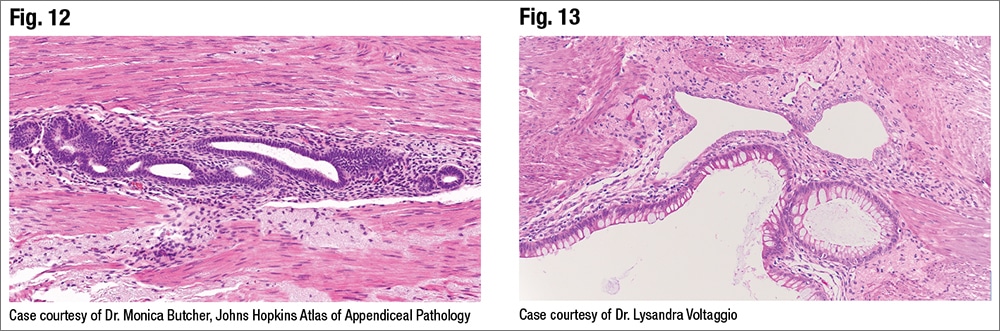
Endometriosis with intestinal metaplasia is one pitfall, Dr. Birkness-Gartman said. “It can potentially mimic a low-grade appendiceal mucinous neoplasm or LAMN.” Associated endometrial-type stroma is a clue, she said. Endometrial-type glands with intestinal metaplasia will label for the intestinal marker. “Luckily, the endometrial stroma retains the expected labeling pattern and is positive for ER and CD10,” she said. In a high-magnification image of endometriosis with intestinal metaplasia (Fig. 13), the endometrial-type stroma surrounding the glands has a spindled appearance and “is a clue to the correct diagnosis in this case” (Vyas M, et al. Pathol Res Pract. 2017;213[1]:39–44).
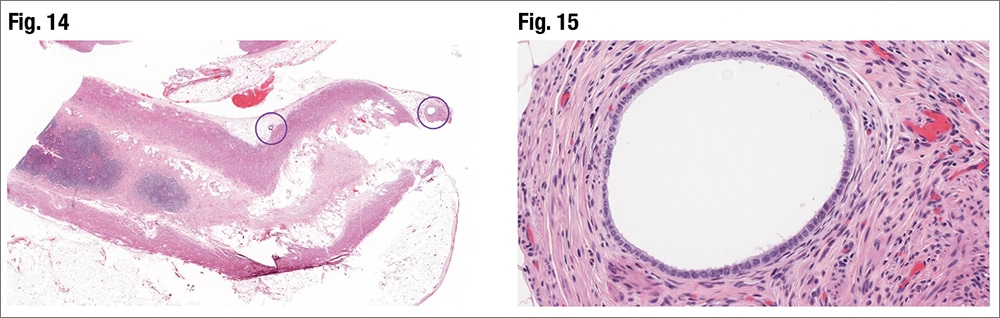
Dr. Birkness-Gartman presented the case of a 40-year-old woman with a history of ampullary adenocarcinoma who underwent a Whipple procedure with en bloc ileocecectomy. Incidental glandular-type structures are seen in Fig. 14 in the periappendiceal adipose tissue and at higher magnification there is no associated endometrial-type stroma (Fig. 15). It is lined by cuboidal epithelial cells that have cilia on the luminal surface. Appendiceal endosalpingiosis is an incidental finding in this case, she said.
Noor, et al., reported finding that the median age of patients with appendiceal endosalpingiosis was 45, and 36 percent of the patients in their study presented with acute appendicitis. “Extra-appendiceal involvement can be seen in 36 percent of patients, but it’s typically not in patients presenting with acute appendicitis,” Dr. Birkness-Gartman said. Histologically, appendiceal endosalpingiosis can involve the muscularis propria or serosa, typically in minute foci, she said. “And we see glands or cystic structures lined by tubal-type epithelium that lack the associated endometrial-type stroma and hemosiderin.”
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
