Amy Carpenter Aquino
September 2018—Qualitative or quantitative testing. Hydrolyze or don’t hydrolyze. Use or don’t use standard cutoffs. These and other decisions in toxicology testing have taken on new urgency amid the opioid crisis, which is driving laboratories to change test methods to assess prescription drug compliance and illicit drug use.
“From a provider’s perspective, it’s difficult to provide adequate pain control while avoiding the risk for abuse,” said Athena Petrides, PhD, director of toxicology and assistant director of chemistry at Brigham and Women’s Hospital, in a session at the AACC annual meeting in July. Dr. Petrides, who is also an assistant professor of pathology at Harvard Medical School, told attendees that more than 40 percent of chronic pain patients report feeling inadequately treated for pain.
At Brigham and Women’s Hospital, the laboratory responded to the increased demand for pain toxicology testing—which rose from approximately 750 tests in 2005 to approximately 3,500 tests in 2017—by developing a new assay to assess pain medication compliance.
“It is straight-to-LC-MS/MS definitive testing. We eliminated the immunoassay,” said co-speaker Stacy Melanson, MD, PhD, associate director of clinical laboratories and co-director of chemistry at Brigham and Women’s Hospital. “There are several guidelines, including one from us as laboratory scientists, that support mass spectrometry as the best methodology to assess medication compliance.”
The new assay is the result of the laboratory’s efforts to adapt urine drug testing to provide more guidance to clinicians and to help manage the opioid crisis, said Dr. Melanson, an associate professor of pathology at Harvard Medical School. “We’ve had a journey with urine drug testing and many changes” coinciding with the opioid crisis.
The speakers framed their AACC session as a friendly back-and-forth discussion on best practices for assessing prescription opioid compliance and illicit drug use. Dr. Petrides took the stance that urine is the preferred specimen for testing while Dr. Melanson defended oral fluid as the specimen of choice. The speakers also argued the merits of quantitative versus qualitative testing, hydrolysis, and standard cutoff limits. “These are all issues that are up for debate,” Dr. Petrides said.
Recent guidelines recommend urine drug testing as a risk assessment tool to detect the presence of prescribed medication as evidence of regimen adherence and to identify unauthorized substances, Dr. Petrides said. “Urine is considered to be the specimen type of choice due to the wider window of detection and the noninvasive way to collect a specimen,” she said, adding: “Oral fluid, however, is increasingly discussed as an alternative to urine.”
The stakes have never been higher for those who manage chronic pain patients. CDC data show that between 59,000 and 65,000 drug overdose deaths occurred in 2016, outnumbering peak deaths from car crashes, HIV, or firearms in any other year, Dr. Petrides said. At least half of all opioid-related overdose deaths reported in 2016 involved a prescription opioid.
One bright spot in the CDC’s prescription opioid overdose data—the decrease in prescription opioid medication rates between 2006 and 2016—was overshadowed by the increase in average days of supply from 13 in 2006 to 18 in 2016, an overall increase of 35.7 percent. “So that means that patients now have more pills in their house,” Dr. Petrides said.
The laboratory at Brigham and Women’s detected significant levels of prescription opioid diversion and illicit drug abuse in its patient population. “We saw 14.7 percent of patients that were potentially diverting their medication, and 28.7 percent of patients were positive for non-prescribed or illicit drugs,” Dr. Petrides said. The synthetic opioid fentanyl is a growing concern. U.S. Drug Enforcement Agency data showed more than 30,000 fentanyl seizures in 2016, almost double the number in 2015, she said. “We’re getting a high positivity rate for fentanyl in our patient population.”

Dr. Petrides
Requests for pain toxicology panels from pain management physicians at Brigham and Women’s declined in recent years while requests from non-pain management physicians were on the rise. “Anecdotally, what we’ve heard is that testing is shifting to the primary care physicians because they see the patient more frequently and are taking over their management,” she said. The clinicians who regularly order pain toxicology tests and interpret the results are “no longer the population we had at the beginning of this epidemic.” Clinicians with less experience in interpreting pain toxicology results may require more guidance from the laboratory.
The previous toxicology panel offered at Brigham and Women’s was a hybrid, Dr. Petrides said. Amphetamines, buprenorphine, cocaine metabolite, fentanyl, THC, barbiturates, tramadol, 6-acetylmorphine, EDDP, and methadone were tested by immunoassay, which offered a large test menu and fast turnaround time.
The platform’s advantages did not overcome its challenges when testing for benzodiazepines and opioids. The lack of specificity in the immunoassay for these classes of drugs in particular required definitive testing by liquid chromatography tandem mass spectrometry (LC-MS/MS). “We were doing immunoassay for some drugs and sending out the positive results to a reference laboratory for confirmation and upfront definitive testing for opioids and benzodiazepines,” Dr. Petrides said.
Data showed a high false-positive rate for many drugs screened by immunoassay, specifically for 6-acetylmorphine, amphetamines, fentanyl, and buprenorphine. “We had an issue,” she said.
The laboratory’s solution was to “create one big definitive testing panel” and test for all prescribed and illicit substances in-house by mass spectrometry. The panel reflected a compromise between the speakers’ positions on the critical components of a definitive testing panel, which Dr. Petrides described as quantitative versus qualitative testing, hydrolysis, and cutoff levels.
“For the sake of this debate, I am going to support reporting qualitative results, performing the hydrolysis step, and using standard cutoffs,” Dr. Petrides said, noting that the views she and Dr. Melanson were going to express during the session were for debate purposes only.
Dr. Petrides presented the case of a 37-year-old female patient prescribed Dilaudid (hydromorphone) for chronic pain. After three months of tracking the patient’s urine hydromorphone levels to assess compliance, the provider called the lab to confirm a suspicion that the patient was not taking her medication. The patient’s urine creatinine levels varied as well. “The results are going up and down, and the clinician is thinking that the patient isn’t really taking it as prescribed,” Dr. Petrides said.
Asked if the test results could be used to determine whether the patient was taking her medication as prescribed, most in the session said no. Dr. Petrides agreed. “Urine drug testing has many variables to determine what the measured drug response is going to be,” she said. “Drug interactions is one; you could be competing for binding to enzymes with these drugs, so the metabolism of that drug isn’t happening as rapidly as you would expect.” Adherence, which is the question in this case, is another.
Other factors to consider: urine adulteration caused by drinking large amounts of water to dilute the urine and mask the presence of the drug; genetic variation if the patient has alterations in the cytochrome P450 enzymes or glucuronosyltransferases (UGT) that cause a different metabolic pattern or conjugation of the drugs; a clinical diagnosis, such as a kidney or liver disease, which could affect results; dose management; and the half-life of the drug—“the most important thing here.”
“I think qualitative testing is the way to go in this case to avoid confusion,” Dr. Petrides said. “You want to avoid the misinterpretation and assumption that you can use these results to determine dose and timing, which is what the physicians are trying to do.” If the question is one of compliance, “why do you need those quantitative numbers? Isn’t the fact that the drug is there evidence enough?”
Qualitative testing requires fewer calibrators, and assay validation is less laborious, she added.
Dr. Petrides made the case for performing the hydrolysis step, which involves incubating the sample to remove the glucuronide group, and sometimes the sulfate group, in order to measure total drug levels instead of the different metabolites—conjugated metabolites—and the primary drug. “You increase your detection sensitivity because you have a larger pool now and it avoids false-negatives,” she said.
Adding the hydrolysis step also results in fewer drugs and their metabolites in the testing panel. “If you have all the results listed for the different glucuronides, it’s going to be a gigantic list and it will be very difficult for clinicians to go through and read every single one,” she said. By using a panel with appropriate metabolites, “you will make interpretation for clinicians easier and allow them to better assess compliance.”
 In the past, for example, noroxycodone was not included in their panel. “It was difficult to assess whether the oxymorphone result was due to oxycodone ingestion or oxymorphone ingestion. It can be either one. By having noroxycodone, you’re able to differentiate that,” Dr. Petrides said.
In the past, for example, noroxycodone was not included in their panel. “It was difficult to assess whether the oxymorphone result was due to oxycodone ingestion or oxymorphone ingestion. It can be either one. By having noroxycodone, you’re able to differentiate that,” Dr. Petrides said.
With oxycodone and oxymorphone in the panel, if the patient is prescribed oxycodone, “in our patient population that would be 31 percent of the positive results.” Adding noroxycodone raised the positivity rate to 36 percent, “and you’re definitely sure that that comes from oxycodone metabolism.”
“This is showing the confidence in your interpretation.”
Dr. Petrides shared another example from her laboratory to support the use of standard cutoffs. “We have an assay that detects benzoylecgonine down to 5 ng/mL—you can go that low—and we had a positive result. The clinician called us and said, ‘My patient is adamantly saying they did not take cocaine. Please send it to another lab.’” Brigham and Women’s sent the specimen to another lab, which had a cutoff of 50 ng/mL, and the result came back negative. “That causes some suspicion of how accurate our results are in our lab. If we all use standard cutoffs, we can consistently assure clinicians that these methods are actually valid for testing their population.”
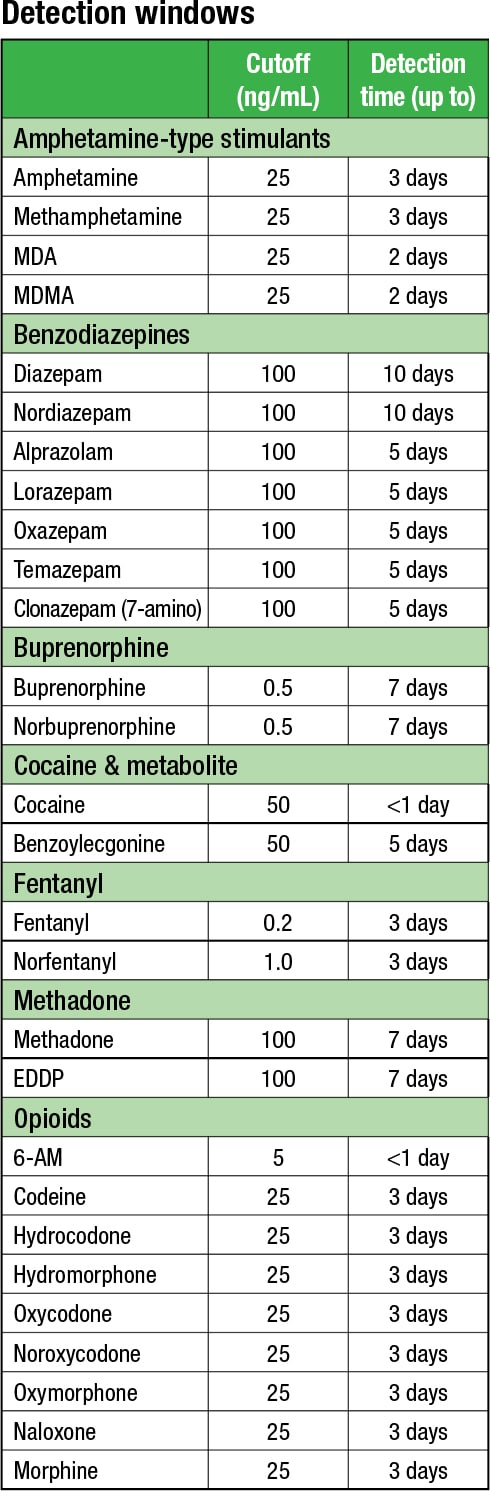
Scientific data exist defining detection windows with use of standard cutoffs, she said. “Although that can vary between individuals, at least you have a ballpark of when the patient might have taken this drug,” which helps the laboratory answer a common question from providers: Was the cocaine strongly or weakly positive? “We can’t answer those questions if we have very, very low cutoffs that we don’t have any data around.”
Laboratories with standard cutoffs would be able to use the accepted detection windows for the different types of drugs, Dr. Petrides said.
Dr. Melanson argued that laboratories should report results quantitatively, not hydrolyze, and use the lower limit of quantitation.
She presented the case of a 54-year-old chronic pain patient with a history of substance abuse managed with methadone. The provider ordered the pain toxicology panel to assess compliance, and results showed that methadone and EDDP (methadone metabolite) were detected, reported qualitatively. Urine creatinine was normal. “If you had those results and your clinician called, would you say this patient is compliant?” Dr. Melanson agreed with the majority of session attendees who answered yes.
But what if the laboratory provided quantitative results? Dr. Melanson asked. “Same patient, but the methadone was sky high, greater than the reporting limit of your assay. There was EDDP there, but it was right at the cutoff, about 5 ng/mL, so both were detected but the parent compound was significantly higher. The creatinine was still normal. If you have these quantitative results in front of you and the clinician called, would you assume this patient is compliant with their medication?”
Quantitative results are better to assess whether the patient is simulating compliance, she said. “In this case, it’s highly suggestive that the patient was dropping the methadone pill directly into their urine so they would get a positive result for methadone.” The low level of EDDP showed that the patient took the prescribed methadone at some point but was currently not compliant.
Quantitative results also allow laboratories to normalize results to urine creatinine, which is helpful for monitoring THC or other drugs the clinician would like to see decrease over time. “If results are not normalized, you might see the results for THC continue to go up,” Dr. Melanson said. “But maybe the urine is getting more concentrated leading to higher results and in fact the patient has stopped using THC. If you normalize to creatinine, you can tell the difference and the clinician can more accurately determine if results are going down over time.”
With quantitative results, the laboratory can also assess whether a drug is present simply because it is an impurity in one of the drug formulations. “Morphine may have a bit of codeine, oxymorphone may have a little bit of oxycodone in it. That wouldn’t be consistent with the patient metabolizing the compound,” she said. The amount of the impurity is usually less than 0.1 percent of the parent drug or the formulation prescribed. Having quantitative results allows the laboratory to “feel pretty comfortable that this is actually due to an impurity and they have not taken an additional drug.”
Dr. Melanson argued against performing hydrolysis by presenting the disadvantages: It is time-consuming and prolongs turnaround time, chemical hydrolysis can degrade opiate and benzodiazepine drugs, and enzymatic hydrolysis can be incomplete and even reduce nordiazepam to oxazepam. “It’s better not to hydrolyze for these limitations and include the glucuronides” for more accurate assessment of opioid prescription compliance, she said.

Dr. Melanson
Dr. Melanson disagreed that hydrolysis was necessary for better sensitivity. “Assays are very good now. If we go down in the lower limit of quantitation, assays will be sensitive enough to measure both the free and glucuronidated drugs.”
She presented data showing that adding the glucuronides helped the laboratory better assess whether a patient was taking prescribed morphine. “We used to measure only morphine and the minor metabolite hydromorphone to assess compliance,” she said. Adding the glucuronides, which are present in all patients taking morphine, resulted in an increase in the positivity rate, according to the data, and improved detection of compliance (Gencheva R, et al. Clinical benefits of direct-to-definitive testing for monitoring compliance in pain management. Pain Physician, in press).
The lower limit of quantitation (LLOQ) “increases the positivity rate particularly for illicit drugs, which are concerning in all patient populations,” Dr. Melanson said. It also will help reduce the incidence of false-negatives. “You won’t be as affected by patients who have dilute urine or matrix effects.”
The data showed increased detection of illicit drugs when the laboratory used the LLOQ. “It increased the positivity rate for all combinations: heroin and fentanyl, cocaine and fentanyl, cocaine and heroin, and morphine and fentanyl. We were better able to identify these patients for the clinicians when we use the LLOQ,” Dr. Melanson said.
Brigham and Women’s laboratory leaders compromised on the points of debate and went live with their new LC-MS/MS testing panel in August 2017. “We are detecting 37 drugs and metabolites, and these were determined in conjunction with our clinicians,” given the patient population and what drugs are prescribed, Dr. Melanson said.
“We went with lower cutoffs and we decided not to perform hydrolysis,” she said. “It was an additional three hours, so we added the glucuronides instead.”
Eliminating the immunoassay saved Brigham and Women’s, which already had the mass spectrometer, about $100,000 in reagents and send-out costs. The laboratory was also able to remove an analyzer that had been dedicated to those immunoassay drug screens.
The testing panel reflects further compromise between reporting quantitative and qualitative results, Dr. Melanson said. “We actually do think that qualitative results are sufficient in most cases, so the majority of new analytes are reported qualitatively.” If the results do not fit the clinical picture or seem suspicious, the laboratory “can always reflex to a quantitative result.”
The laboratory stayed with quantitative results for opioids and benzodiazepines that were already being tested in-house. “We had been doing them since 2010, so the clinicians were used to getting quantitative results,” she explained. Clinicians also preferred quantitative results for buprenorphine in particular. “It is a drug for which we see a lot of simulated compliance, and there are published papers showing that you can use the ratios of parent to metabolite as well as the naloxone to determine if the patient is compliant.”
Since there is no hydrolysis step and therefore many drugs and metabolites are reported, Dr. Melanson said the laboratory is considering systematically interpreting results for clinicians based on the patient medications prescribed at the time of collection. “We feel it’s important to help our providers interpret these,” she said, adding that the laboratory is currently studying how well clinicians are interpreting results since the implementation of the new assay.
“If we get an email from a provider, we will answer on a case-by-case basis to try to help them assess compliance,” she said. Adding a comment to some or all results may also be helpful. In an example of a patient who was prescribed clonazepam and buprenorphine, the results showed acceptable levels of the parent compound clonazepam and the metabolite 7-aminoclonazepam, but high levels of buprenorphine and very low levels of the metabolites. The patient also had very high levels of naloxone, which suggested the patient was not taking the buprenorphine as prescribed. “We might provide a comment to alert the clinician that the patient most likely dropped the buprenorphine pill directly into their urine,” she said.
Fentanyl and its metabolite, morphine, high levels of the morphine glucuronides, and hydromorphone were also detected. “All in all, this suggests they’re taking fentanyl and morphine,” Dr. Melanson said. “We might add a comment that says, ‘Suggestive of fentanyl and morphine use, prescriptions for which were not found in the medical record,’” and that those results could be from heroin use.
Drs. Melanson and Petrides plan to publish their findings on how well the clinicians are interpreting results once the study is complete.
In the debate over oral fluid versus urine as the specimen of choice, Dr. Melanson referred to the laboratory’s study, which showed that amphetamines and the heroin metabolite 6-acetylmorphine were detected at higher rates in oral fluid. She also supported oral fluid for being noninvasive, less likely to be adulterated, more effective at detecting drugs in real time, and resisting poppy products and overhydration.
Adapted from Petrides AK, et al. Clin Chim Acta. 2018;481[6]:75–82.
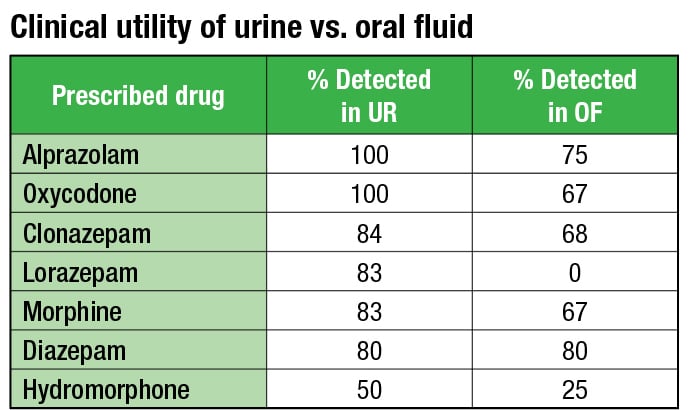
Dr. Petrides noted the disadvantages of testing oral fluid: small specimen volume, dependence on collection device and person performing collection, and unknown windows of detection. The laboratory’s study showed that benzodiazepines, buprenorphine, and cocaine were detected better in urine compared with oral fluid, she said.
Drs. Melanson and Petrides reached a compromise by reviewing patient records to determine the performance of each matrix for prescribed medications. “For prescribed medications in the study—alprazolam, oxycodone, clonazepam, lorazepam, morphine, diazepam, and hydromorphone—the detection rates were higher in urine than oral fluid,” Dr. Petrides said, adding that it therefore may be better to use urine in a pain management setting but not in an addiction setting.
They looked more closely at the heroin metabolite 6-acetylmorphine, which gets metabolized to morphine. 6-AM was better detected in oral fluid, in accordance with its biochemical properties. Their data showed that morphine did not have a preference for the matrix in which it was detected.
“What we hypothesized was that where you would find the morphine is dependent on the time of collection in relation to the time of ingestion,” Dr. Petrides said.
Plotting the oral fluid-to-urine ratio of morphine concentration revealed a time course. In oral fluid, there is a bell-shaped curve. “When you see a low result in oral fluid, it can either be due to recent use or it can be due to remote use. It’s hard to say whether if you get a positive result for 6-AM in oral fluid exactly when the patient took it,” Dr. Petrides said. “So oral fluid is the preferred matrix for 6-AM and amphetamine. But using a ratio of oral fluid-to-urine morphine could assist with interpreting 6-AM results.”
The final proposed testing algorithm settled on oral fluid as the preferred matrix for 6-AM and amphetamines, and urine for 7-aminoclonazepam, lorazepam, oxazepam, hydromorphone, oxymorphone, buprenorphine, and cocaine. More studies are needed to determine the preferred matrix for fentanyl, tramadol, MDMA/MDA, and methadone.
Dr. Petrides closed the session on a note about continued challenges from clinicians. A 45-year-old woman with advanced cervical cancer was prescribed oxycodone for pelvic pain. When a urine toxicology panel (by LC-MS/MS) revealed the presence of benzoylecgonine, a cocaine metabolite, she denied using cocaine. The patient suggested to her physician that her oral fluid contact with her dog, which had been prescribed the antibiotic clindamycin, caused her urine to test positive for cocaine. The clinician requested a test for clindamycin for the patient.
“This was a real case,” Dr. Petrides said. “It was pretty interesting to try to convince the clinical team that this could not possibly ever happen.”
Amy Carpenter Aquino is CAP TODAY senior editor.