Jennifer A. Brainard, MD
Zaibo Li, MD, PhD, MBA
August 2019—The CAP has a long-standing commitment to education in cytopathology, with a number of organized educational offerings in gynecologic and nongynecologic cytopathology. The Interlaboratory Comparison Program in nongynecologic cytopathology (NGC Education) was started in 1997 and the Interlaboratory Comparison Program in fine-needle aspiration glass slide education (FNAG) in 2010. These programs are strictly educational and not graded or used for proficiency testing. Semiannual (FNAG) and quarterly (NGC) mailings include four or five cases. For each case, glass slides generally stained with a Diff-Quik and/or Pap stain are provided. The corresponding clinical histories are supplied, and some cases have accompanying ancillary studies such as cell block preparations or immunohistochemical stains, which can be accessed from the CAP website.
The result forms for NGC and FNAG consist of three parts. The first part is the general diagnostic category menu, which is divided into five categories: unsatisfactory, benign, atypia/indeterminate/neoplasm, suspicious for malignancy, and malignant. The atypia/indeterminate/neoplasm general diagnostic category was added in 2018 to reflect the inherent biologic uncertainty of some cytologic diagnoses and to support new reporting systems recently adopted in cytopathology. The general category is applied to those lesions in which there is morphologic overlap between neoplasms and non-neoplastic entities (for example, atypia of undetermined significance in thyroid FNA) as well as between benign and malignant neoplasms (for example, basaloid neoplasms of salivary gland).
The second part of the result form is a specific interpretive menu unique to each organ or site. Each interpretation has a dedicated diagnostic N-code. An answer is considered correct from the reporting and benchmarking point of view if it is concordant with the general diagnostic category. The specific diagnostic N-code reflects the best and most specific diagnosis for the case and provides important feedback to the participant.
The third part of the form allows the participant to provide feedback on the technical slide quality by selecting acceptable or unacceptable.
The result form has a preassigned general diagnostic category for each interpretation. This was implemented because participants were not always sure where, in the general category, to place certain lesions. For example, serous or mucinous tumors of the ovary could reasonably be placed in the atypia/indeterminate/neoplasm, suspicious for malignancy, or malignant category depending on their biologic behavior. Placing interpretations under specific categories takes the guesswork out of the exercise and makes the correct category clear to the participant.
As the field of cytopathology has evolved and expanded over the years and with the development of new, standardized, category-based reporting systems, participant choices (specifically N-codes) have also changed to reflect current practice. For example, N-codes have been added to encompass the Bethesda System for Reporting Thyroid Cytopathology as well as the Paris System for Reporting Urinary Cytology. Each time a new terminology gains acceptance, the inventory for that particular organ (all thyroid FNA cases, for example) is removed from circulation and reviewed by members of the CAP Cytopathology Committee and reclassified using the new system. Depending on the number of cases in the program, this process may take more than a year to complete, as the committee meets quarterly. In the near future, salivary gland FNA slides will be removed from the program and reclassified according to the Milan System for Reporting Salivary Gland Cytopathology.
In addition, slides are reviewed and N-codes are potentially revised when diagnostic standards of care in a particular organ system change. For example, lung cytology has evolved dramatically over the past decade. A diagnosis of non-small cell carcinoma is not specific enough in this age of personalized medicine and is no longer the most acceptable diagnosis in most cases of lung carcinoma. The field of lymph node FNA and, specifically, lymphoma diagnosis has also advanced and become more reliant on ancillary testing, including flow cytometry and molecular genetic testing. As a result, the reclassification of lung cases is complete and the reclassification of lymph node cases is near completion. The CAP Cytopathology Committee reviewed all glass slides from these cases, with emphasis placed on the addition of ancillary studies to arrive at a diagnosis that is more specific and meets the diagnostic needs of today’s patients and their treating physicians. These periodic slide reviews also allow for added quality assurance because they allow for removal of slides that are of poor quality.
To provide feedback on slide performance, statistics are generated for each diagnostic category as well as for each slide regardless of the number of responses. The previous four years’ worth of data were reviewed and certain trends were identified. Problematic areas—that is, those that show less than 90 percent participant agreement with the correct general diagnostic category—have been relatively consistent over the past four years. Discrepancies are due to under-calling of malignant cases as well as over-calling of benign and indeterminate cases. Data from the program from 2018 are in Tables 1 and 2. Only those cases with greater than 100 laboratory responses are included in the tables.
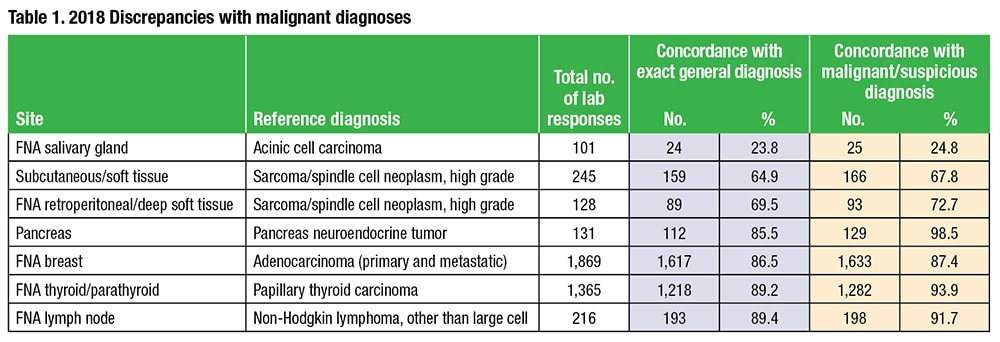
FNA case responses are more often discrepant with the reference diagnosis than other nongynecologic specimen types. Metastases and uncommon primary tumors are also disproportionately misclassified. This may be related to difficulties accessing or interpreting electronically available ancillary studies. Cases from certain organ systems, such as thyroid, breast, lymph node, salivary gland, and soft tissue, have historically been the most problematic. As may be expected, aspirates from sites with indeterminate diagnostic categories (i.e. thyroid and salivary gland) tend to have higher discrepant rates, reflective of the interobserver variability that is well established in the cytopathology literature. The Cytopathology Committee is closely monitoring slide performance to assess the impact of new classification systems on discrepancy rates.
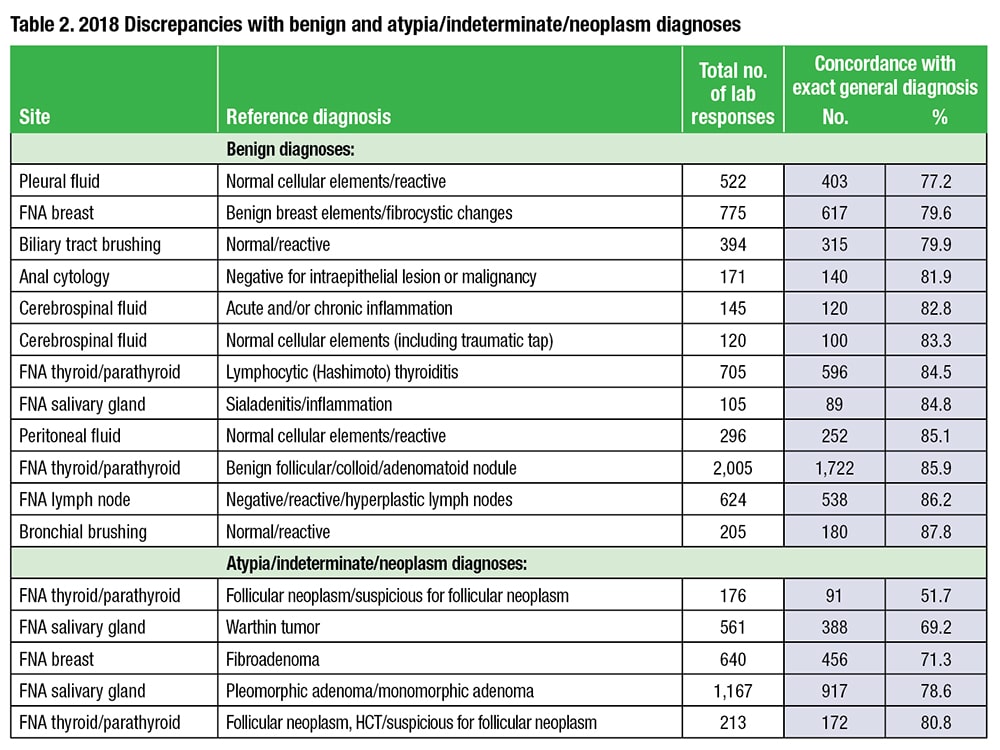 Within the lymph node and soft tissue FNA categories, aspirates from lymphomas and spindle cell lesions, respectively, appear to be the most challenging. Such cases are generally few in number in daily practice and rely heavily on ancillary studies for correct diagnoses. The committee is now in the final phase of reclassifying all lymph node FNAs in the program. These cases will soon be returned to the program. The Cytopathology Committee will continue to monitor discrepant cases to determine if slides reclassified to incorporate updated diagnostic terminology and inclusion of ancillary studies perform better in the program.
Within the lymph node and soft tissue FNA categories, aspirates from lymphomas and spindle cell lesions, respectively, appear to be the most challenging. Such cases are generally few in number in daily practice and rely heavily on ancillary studies for correct diagnoses. The committee is now in the final phase of reclassifying all lymph node FNAs in the program. These cases will soon be returned to the program. The Cytopathology Committee will continue to monitor discrepant cases to determine if slides reclassified to incorporate updated diagnostic terminology and inclusion of ancillary studies perform better in the program.
Members of the Cytopathology Committee are committed to providing valuable education in cytopathology. The committee uses data generated from these slide programs to provide additional educational content in diagnostically challenging areas and works diligently to provide an up-to-date and worthwhile educational experience, reflective of the needs of today’s practice. We value and use participant feedback on the educational experience, including quality of slides and ancillary material, to further enhance the Interlaboratory Comparison Programs.
Dr. Brainard, vice chair of the CAP Cytopathology Committee, is vice chair of cytology operations, Cleveland Clinic. Dr. Li, a member of the committee, is an associate professor of pathology, Ohio State University Wexner Medical Center, Columbus.