First synoptic for cytopathology
Sana O. Tabbara, MD; Lananh Nguyen, MD
Abha Goyal, MD; George G. Birdsong, MD
August 2022—The protocol for the reporting of cervicovaginal cytology, the first in a series of CAP cytopathology protocols, became available for use in a synoptic format on June 22 (https://capatholo.gy/3uHusnU).
This protocol is a collaborative effort, based on input from past and present members of the CAP Cytopathology Committee and prepared in conjunction with the CAP Pathology Electronic Reporting Committee. It was presented via webinar to the CAP House of Delegates on March 31. A two-week open comment period followed; all comments were reviewed and appropriate changes were incorporated into the protocol. Although the protocol is in a synoptic format, it is meant to replace existing gynecologic cytopathology/Pap test reports and not be an add-on to the report. The protocol will not be a requirement for accreditation at this time.
The aim of this comprehensive protocol is to improve the completeness, clarity, and portability of Pap test reporting while being mindful of the wide range of practice settings in which the data in the report is generated and to which it is disseminated. This protocol uses the standardized Bethesda System for Reporting Cervical Cytology1 and incorporates clinical history and ancillary testing results that may prove crucial in managing the patient. For instance, it includes the history of dysplasia/malignancy/ HPV infection as well as details on concurrent HPV testing, if any. Including this data in the report will facilitate risk-based management of patients, as recommended by the 2019 American Society for Colposcopy and Cervical Pathology management consensus guidelines.2 The protocol also features HPV vaccination history, which is important information in understanding the impact of the vaccine and possibly modifying the screening strategy in vaccinated individuals in the future.
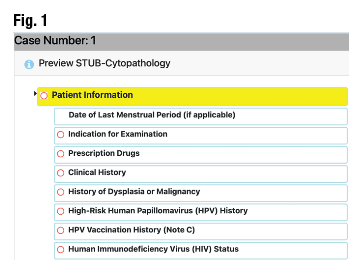
The components of the protocol include patient information, preanalytical examination of the specimen, interpretation (based on the Bethesda System), and ancillary testing. The protocol has required fields and some optional fields to be consistent with other synoptic reports. Fig. 1 shows the first field, “patient information,” and below it are subfields, which include the optional field “date of last menstrual period (if applicable)” and required fields “indication for examination,” “prescription drugs,” “clinical history,” and others. Fig. 2 is an example of a subfield, “high-risk human papillomavirus (HPV) history,” showing a thorough list of specific information to be entered—for example, specific HPV genotypes. Fig. 3 shows the third field, “interpretation,” an example of an explanatory note as seen in subfield “specimen adequacy” and designated “(note D).” The protocol also takes into consideration the introduction of additional testing recommendations and modalities that may be applied more widely in the future, as seen in the “ancillary testing” field in Fig. 4.3,4 We encourage all readers to access and explore the synoptic in its full detail.

This protocol can be used as a guide for trainees and pathologists who may encounter only a limited number of Pap tests in their practice. As a replacement for the current final report, and like synoptic reports that supplement surgical pathology reports, the goal is to have this protocol adapted to laboratory information systems to facilitate its use and make it easier to provide reproducible and extractable data. As such, efforts are underway to introduce this format to LIS vendors. The committees hope this is a first step in providing a framework for a more comprehensive cervicovaginal Pap test report to improve quality and interoperability, with revisions provided in the future as needed.

The content of the protocol represents the consensus opinion of the CAP Cytopathology Committee and the CAP Pathology Electronic Reporting Committee. The committees recommend that all available elements be included.
- Nayar R, Wilbur DC, eds. The Bethesda System for Reporting Cervical Cytology: Definitions, Criteria, and Explanatory Notes. 3rd ed. Springer; 2015.
- Perkins RB, Guido RS, Castle PE, et al. 2019 ASCCP risk-based management consensus guidelines for abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2020;24(2):102–131.
- Fontham ETH, Wolf AMD, Church TR, et al. Cervical screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin. 2020;70(5):321–346.
- U.S. Preventive Services Task Force. Screening for Cervical Cancer: U.S. Preventive Services Task Force Recommendation Statement. JAMA. 2018;320(7):674–686.

Dr. Tabbara is director of cytopathology, Moffitt Cancer Center, and professor of oncologic sciences, USF Morsani College of Medicine, Tampa; Dr. Nguyen is director of cytopathology and assistant professor, Department of Laboratory Medicine, Unity Health Toronto, University of Toronto; Dr. Goyal is associate professor of clinical pathology and laboratory medicine, Weill Cornell Medicine-New York Presbyterian Hospital; and Dr. Birdsong is director of anatomic pathology and professor, Department of Pathology and Laboratory Medicine, Emory University School of Medicine at Grady Hospital, Atlanta. Dr. Tabbara is chair of the CAP Cytopathology Committee, Dr. Nguyen is vice chair, and Dr. Goyal is a member. Dr. Birdsong is a former member of the CAP Pathology Electronic Reporting Committee and of the Cytopathology Committee.