
Esther Diana Rossi, MD, PhD
Daniel F. I. Kurtycz, MD
William C. Faquin, MD, PhD
 May 2018—The Milan System for Reporting Salivary Gland Cytopathology was published Jan. 31 and is an important step toward standardizing the reporting of salivary gland fine needle aspiration.1
May 2018—The Milan System for Reporting Salivary Gland Cytopathology was published Jan. 31 and is an important step toward standardizing the reporting of salivary gland fine needle aspiration.1
A large body of literature has demonstrated that FNA is an effective method for the initial evaluation of salivary gland masses, but until this year there was no uniform, widely accepted reporting system. The complexity of salivary gland cytology poses unique challenges that demand a standardized approach to communication of diagnostic information between pathologists and treating clinicians. Establishing a common reporting language promotes education and research in salivary gland cytology just as other diagnostic cytology systems have done in their respective areas of cytopathology. Creation of such reporting systems is a natural consequence of the maturation of evidence-based literature and clinical experience. Thus it is that the first atlas for salivary gland cytopathology is now available.

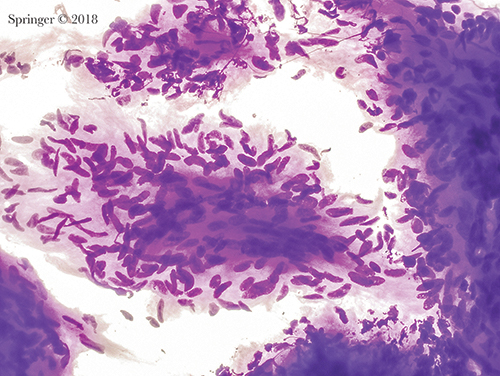
Non-neoplastic. Amylase crystals are non-birefringent crystalline structures with rectangular, needle-shaped, rhomboid, and platelike shapes. They are most commonly associated with non-neoplastic inflammatory conditions as in this case (smear, Papanicolaou stain).
The cytomorphology of a variety of salivary gland tumors has been defined over decades of practice. Unique features of a number of salivary gland lesions, including the cytomorphologic overlap of some benign neoplasms and low-grade carcinomas, have been well described. The accuracy of salivary cytology is high for the diagnosis of the most common salivary gland tumors such as pleomorphic adenoma and Warthin tumor, but the specificity for subtyping a particular neoplasm shows a wide range (48 to 94 percent) depending on tumor type. Accuracy is generally high for distinguishing benign and low-grade neoplasms from high-grade carcinomas.2–13 It is useful to remember that the nature and types of a given salivary gland lesion (neoplastic and non-neoplastic) vary depending on anatomic site. The rate of malignancy varies from 20 to 25 percent in the parotid gland, from 40 to 50 percent in the submandibular gland, and up to 80 percent in minor salivary glands of the oral cavity.

Non-neoplastic. This aspirate of granulomatous sialadenitis shows a large group of epithelioid histiocytes; an infectious agent should be excluded (smear, Papanicolaou stain).
The overall effectiveness of salivary gland FNA at a given institution depends on a number of factors, including the use of ultrasound guidance, rapid on-site evaluation, the cytologic preparation used (liquid-based, alcohol-fixed smears, and air-dried smears), and technical and diagnostic experience. Optimizing these factors enhances the diagnostic utility of salivary gland FNA. Various aspects of the lesion, such as tumor subtype, lesional heterogeneity, and presence of cystic elements, will also influence the diagnostic accuracy of the FNA.
There had been no uniform classification system for reporting salivary gland FNAs. Thus, the American Society of Cytopathology with the support of the International Academy of Cytology established an international working group, composed of more than 40 participants from 15 countries. The group consisted of cytopathologists, surgical pathologists, and head and neck surgeons. Their goal was to establish a tiered reporting system, which has now been designated the Milan System for Reporting Salivary Gland Cytopathology (MSRSGC). The name reflects the first gathering of the core working group during the 2015 annual meeting of the European Congress of Cytology in Milan, Italy.

Non-diagnostic. Non-mucinous cyst contents showing histiocytes, debris, and a few inflammatory cells (smear, Papanicolaou stain).
The Milan System consists of six diagnostic categories (Table, below). It is an evidence-based system that correlates diagnostic categories with risk of malignancy and clinical management. The soft-bound atlas has 10 chapters that contain detailed descriptions of each of the six diagnostic categories of the Milan System. The atlas incorporates explanatory notes and color image FNA examples for each entity. The six diagnostic categories are non-diagnostic, non-neoplastic, atypia of undetermined significance (AUS), neoplasm subclassified into benign and salivary gland neoplasm of uncertain malignant potential (SUMP), suspicious for malignancy, and malignant.
The opening chapter of the atlas describes indications for salivary gland FNA as well as FNA technique, associated preparation methods, and implied risks of malignancy. The final three chapters are dedicated to ancillary testing for FNA, recommendations for clinical management, and histologic considerations.

Pleomorphic adenoma. The stroma lacks the usual fibrillary character and mimics thick mucin (smear, Romanowsky stain).
The Milan System is based on key principles developed for standardized terminologies adopted for other anatomic sites, including the uterine cervix, pancreas, and urinary system. The atlas format is similar to that of The Bethesda System for Reporting Thyroid Cytopathology.14 (See article For thyroid cytopathology, the 2017 Bethesda System.) The objective of the working group was to create a user-friendly system that will promote and standardize communication between cytopathologists and treating clinicians, cyto-histological correlation, and the exchange of information among institutions.

Atypia of undetermined significance. This aspirate contains abundant mucin without any epithelial cells. The differential diagnosis includes a benign mucinous cyst; however, a low-grade mucoepidermoid carcinoma cannot be excluded (smear, Romanowsky stain).
The non-diagnostic category includes samples with significant limitations, often due to scant cellularity or preservation artifact. Also included are samples characterized by nonmucinous cyst contents, aspirates of normal salivary gland tissue only, and aspirates lacking adequate material for evaluation. An online consensus survey opinion was that samples showing only normal salivary gland elements in the context of a defined clinical or radiologic mass should be deemed non-diagnostic.15 This is in keeping with the concept of the “triple test” in that cytologic, radiologic, and clinical findings should be concordant. The non-diagnostic chapter supports radiologic correlation and emphasizes the value of ultrasound guidance for its value in defining and targeting a lesion.
Neoplasm: benign. This aspirate of schwannoma shows a group of bland spindle cells with wispy cytoplasm. The cytoplasmic borders are indistinct. Nuclei are spindle-shaped and display bends or curves (smear, Romanowsky stain).
The non-neoplastic category includes benign, reactive, metaplastic, and inflammatory processes such as acute, chronic, and granulomatous sialadenitis. The risk of malignancy, or ROM, for this category will be low when strict inclusion criteria are used. It is recognized that sampling errors occur, and such errors can be responsible for a non-neoplastic diagnosis when a neoplastic lesion is present. Recommendations are made for close clinical follow-up and radiologic correlation.
Similar to the Bethesda System for thyroid cytopathology, the Milan System strictly defines and limits the FNA cases assigned to its atypical category, AUS (atypia of unknown significance). FNAs classified as AUS samples contain limited atypical features that are indeterminate for a neoplasm. According to Milan criteria and literature experience, AUS cases should account for less than 10 percent of salivary gland FNA samples. In this way, a goal of the AUS category is to reduce the number of false-negative diagnoses in the non-neoplastic category while helping to maintain the significance of the neoplastic category. Cases diagnosed as AUS could be managed by either repeat FNA or conservative surgical resection according to the specific clinical and radiologic contexts of the lesion.
Suspicious for malignancy. This smear is composed of basaloid cells and abundant matrix spheres with a pattern suspicious for adenoid cystic carcinoma (smear, Papanicolaou stain).
There are two different subgroups of neoplasms in the Milan System. The first, termed “benign,” is reserved for cases of benign neoplasms diagnosed based on the presence of established cytomorphologic criteria including classical cases of pleomorphic adenoma and Warthin tumor. A number of other entities, such as benign soft tissue tumors including lipoma and schwannoma, are incorporated into this category. As expected, the ROM for this category should be low (less than five percent). Most benign salivary gland neoplasms such as pleomorphic adenoma are managed by conservative surgical resection, although in selected cases the patient might be followed clinically.

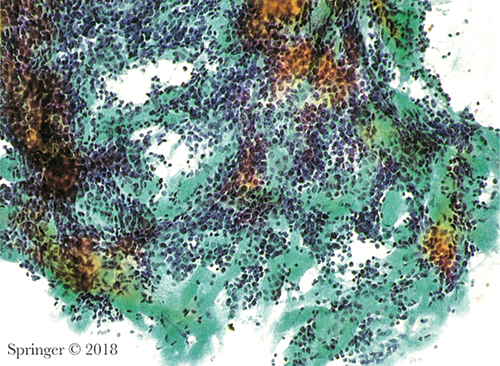
Malignant. Adenoid cystic carcinoma. Aspirates show small high N:C ratio basaloid tumor cells surrounding acellular matrix with a cribriform pattern (smear, Papanicolaou stain).
The second neoplastic group is defined as salivary gland neoplasm of uncertain malignant potential, or SUMP. It consists of FNA specimens that are diagnostic of a neoplasm but for which a diagnosis of a specific entity cannot be made and, importantly, a carcinoma cannot be entirely excluded. A majority of SUMP cases will be cytologically bland cellular neoplasms, neoplasms with atypical features, and low-grade carcinomas. Subsets of the different entities in the SUMP category are included based on basaloid, oncocytic, or clear cell features. Even though entities in the SUMP cytologic category may not have a precise classification, the category defines a ROM of approximately 35 percent and provides important information to help guide clinical management. In the majority of cases, lesions classified as SUMP will typically be managed by conservative surgical resection with negative margins. Currently available ancillary immunohistochemical and molecular studies may allow for more precise classification.

Acinic cell carcinoma. SOX10 immunostain showing strong nuclear expression in the tumor cells in a cell block.
In the suspicious for malignancy (SM) and malignant diagnostic categories, definitions and criteria are analogous to the same categories in other anatomic sites. Lesions classified as SM have features suggestive of malignancy but the sample is either deficient in the quality of the cellular features or the quantity of abnormal cells present. For salivary gland FNAs diagnosed as malignant, criteria are provided to enable cytologists to subclassify the tumors into low-grade and high-grade entities, since these designations have significant implications for patient management. Management of high-grade carcinomas may include radical surgical resection, sacrifice of major nerves, and neck dissection.
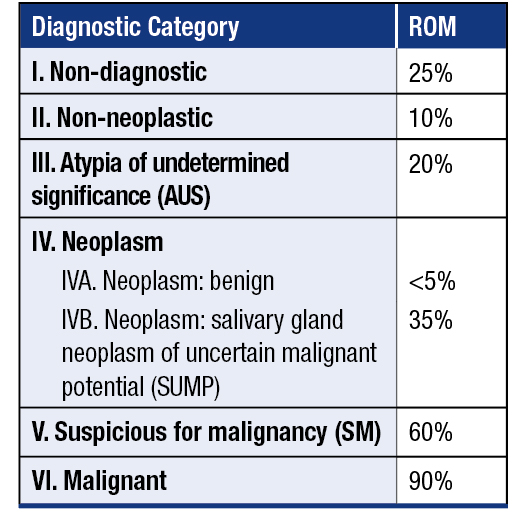
Diagnostic categories and risk of malignancy in The Milan System for Reporting Salivary Gland Cytopathology
The Milan System atlas chapter dedicated to ancillary studies details the use of ancillary techniques, including immunochemistry and molecular testing, and makes clear the role such ancillary tests can play in increasing the overall accuracy and effectiveness of salivary gland FNA.
Efforts are underway to encourage the cytology community to follow the Milan System on Twitter (https://twitter.com/MilanSystem) and Facebook (www.facebook.com/MilanSystem) or the ASC website (www.cytopathology.org) and the Milan System site (www.milansystem.org). There, the latest updates, case examples, and discussions related to salivary gland FNA will be found. The editors are conducting an interobserver reproducibility study with access available through the ASC website. In addition to the print atlas, a Web atlas of the Milan System illustrating numerous examples from each of the diagnostic categories will also be available through the ASC website in the coming months.
- Faquin WC, Rossi ED, eds. The Milan System for Reporting Salivary Gland Cytopathology. Cham, Switzerland: Springer; 2018.
- Ahn S, Kim Y, Oh YL. Fine needle aspiration cytology of benign salivary gland tumors with myoepithelial cell participation: an institutional experience of 575 cases. Acta Cytol. 2013;57(6):567–574.
- Al-Abbadi MA. Pitfalls in salivary gland fine-needle aspiration cytology (author reply). Arch Pathol Lab Med. 2006;130(10):1428.
- Ameli F, Baharoom A, Md Isa N, Noor Akmal S. Diagnostic challenges in fine needle aspiration cytology of salivary gland lesions. Malays J Pathol. 2015;37(1):11–18.
- Chakrabarti S, Bera M, Bhattacharya PK, et al. Study of salivary gland lesions with fine needle aspiration cytology and histopathology along with immunohistochemistry. J Indian Med Assoc. 2010;108(12):833–836.
- Colella G, Cannavale R, Flamminio F, Foschini MP. Fine-needle aspiration cytology of salivary gland lesions: a systematic review. J Oral Maxillofac Surg. 2010;68(9):2146–2153.
- Kim BY, Hyeon J, Ryu G, et al. Diagnostic accuracy of fine needle aspiration cytology for high-grade salivary gland tumors. Ann Surg Oncol. 2013;20(7):2380–2387.
- Krane JF, Faquin WC. Salivary Gland. In: Cibas ES, Ducatman BS, eds. Cytology: Diagnostic Principles and Clinical Correlates, 4th ed. Philadelphia: Saunders Elsevier; 2014.
- Griffith CC, Pai RK, Schneider F, et al. Salivary gland tumor fine-needle aspiration cytology: a proposal for a risk stratification classification. Am J Clin Pathol. 2015;143(6):839–853.
- Rossi ED, Wong LQ, Bizzarro T, et al. The impact of FNAC in the management of salivary gland lesions: institutional experiences leading to a risk-based classification scheme. Cancer Cytopathol. 2016;124(6):388–396.
- Schmidt RL, Hall BJ, Layfield LJ. A systematic review and meta-analysis of the diagnostic accuracy of ultrasound-guided core needle biopsy for salivary gland lesions. Am J Clin Pathol. 2011;136(4):516–526.
- van der Schroeff MP, Terhaard CH, Wieringa MH, Datema FR, Baatenburg de Jong RJ. Cytology and histology have limited added value in prognostic models for salivary gland carcinomas. Oral Oncol. 2010;46(9):662–666.
- Wang H, Fundakowski C, Khurana JS, Jhala N. Fine-needle aspiration biopsy of salivary gland lesions. Arch Pathol Lab Med. 2015;139(12):1491–1497.
- The Bethesda System for Reporting Thyroid Cytopathology, 2nd ed. Ali S, Cibas ES, eds. Cham, Switzerland: Springer; 2017.
- Rossi ED, Faquin WC, Baloch Z, et al. The Milan System for Reporting Salivary Gland Cytopathology: analysis and suggestions of initial survey. Cancer Cytopathol. 2017;125(10):757–766.
[hr]
Dr. Rossi is in the Division of Anatomic Pathology and Histology, Catholic University of Sacred Heart, and a professor in the Agostino Gemelli School of Medicine, Rome. Dr. Kurtycz is medical director, Wisconsin State Laboratory of Hygiene, and a professor in the Department of Pathology and Laboratory Medicine, University of Wisconsin School of Medicine and Public Health, Madison. Dr. Faquin is director of head and neck pathology, Massachusetts General Hospital, and professor of pathology, Harvard Medical School, Boston. Drs. Rossi and Faquin are editors, and Dr. Kurtycz is an associate editor, of The Milan System for Reporting Salivary Gland Cytopathology.