Anne Paxton
October 2019—You may not be curling up next to the fire with a cup of hot chocolate to read your copy of the new Digestive System Tumours, part of the World Health Organization Classification of Tumours Series. You’re more likely to have it sitting nearby at work with dog-eared pages and a cup of coffee on it, says Ian Cree, MB ChB, PhD, head of the WHO Classification of Tumours Group and editorial board chair of the latest and fifth edition. Still, as essential reference guides in medicine go, the freshly minted 635-page tome, released worldwide in June, is a ravishing picture book.
Featuring more than 1,000 high-resolution color graphics, Digestive System Tumours, the first volume of the fifth edition of the WHO series known as the Blue Books, brings a noticeable improvement in image quality and graphic design over the fourth edition, published in 2008. The book’s two-column layout, replacing the former three-column design, allows for enlarged images throughout. And this book is the first to be produced in both a print version and an online subscription version that includes whole-slide imaging.

Dr. Washington
More important, the book has been rewritten and reorganized to incorporate new tumors, new information about how each tumor behaves, and other significant advances in classification since the 2008 edition. “The new edition was a worldwide, collective project that brought together pathologists from Asia, South America, Europe, North America, Australasia, and Africa to collaborate using the best available evidence and practices,” says Mary Kay Washington, MD, PhD, professor of pathology, microbiology, and immunology at Vanderbilt University Medical Center and a standing member of the WHO series editorial board.
Now that the new book is available, the WHO board hopes people can start using the terminology immediately, Dr. Washington says.
Classification is important because it creates the international standards that underpin diagnoses of all tumor types in all cancers, says Dr. Cree, who is a pathologist with the International Agency for Research on Cancer in Lyon, France, publisher of the WHO Classification of Tumour Series. “It means that you can compare data worldwide from different health care systems very easily. If you have a stomach cancer in the U.S. or in Europe or in Japan, it will be the same. You can therefore compare clinical trial results and be confident that patients are getting similar, if not identical, diagnoses from pathologists across the world.”
The fourth edition of the WHO series set a whole new standard and raised the bar considerably from the third edition, Dr. Cree says. “And we are honestly trying to do the same with the fifth edition.” The new online subscription feature, for example, is intended not only to make user access easier but also to show significantly more content. “We have a whole-slide image for each diagnosis in the book. Whole-slide images allow us to get an overview of the entire section of the slide right down to the individual cells and see what is going on.” In addition, each paper in the book has a direct online link to the evidence that underpins the paper, he notes.
The large amount of genomic information in this new edition of Digestive System Tumours reflects how necessary molecular data are becoming in diagnosing some tumors, though by no means all, Dr. Cree says. “There is an increasing amount of information that is of very considerable use. If you look at cancer incidence across the U.S., you would find that the bulk of patients have tumors within the top 10. Those are the ones we tend to use quite a bit of molecular information with.”
From the chapter “Genetic tumour syndromes of the digestive system,” juvenile polyposis syndrome.

Gastric juvenile polyps.
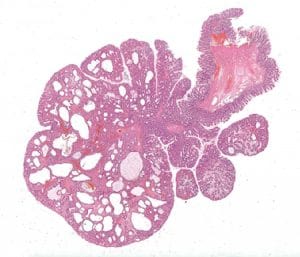
Colonic juvenile polyp. An example from a patient with juvenile polyposis syndrome, characterized by an increase of the stroma and cystically dilated crypts.
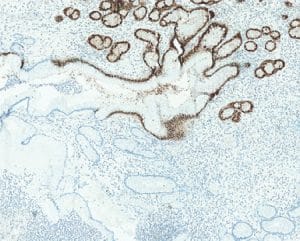
Gastric juvenile polyp. SMAD4 loss in a polyp from a patient with a germline SMAD4 mutation.
The molecular data are also proving that appearances can be deceiving. “We are finding that certain tumors turn out to be the same genetically despite the fact that they look sometimes quite different. We are finding others that look the same but are actually quite different. So the data are increasing our ability to classify and therefore to diagnose,” Dr. Cree says. Among other milestones, this edition of Digestive System Tumors is the first in which certain tumor types are being described as much by molecular phenotype as by histological characteristics. “We have some tumor types where, without the molecular information, you cannot make the diagnosis. It is certainly a new departure for us to put together that information with the standard histopathology.”
The incorporation into the book of the many advances in understanding the genetic drivers of tumors is one of the book’s most important new features, Dr. Washington says. “We probably aren’t to the point of using molecular classification for most GI tumors yet, but we are including a lot more information on the basic genetics.”
A team effort was behind the classifications in the fifth edition of the WHO series. “One thing we did is set up an editorial board. We didn’t have one before,” says Dr. Cree, who asked that CAP members be included on the board when he was appointed to lead it. “We have pathologists and, increasingly, other clinical colleagues on those boards and they consider the evidence that is collected by up to 200 authors for each book. I hope we have not made the team work too much harder, but we have certainly made them work faster. The writing phase is done much more quickly, we are doing a lot of work in parallel to speed up the production phase, and we are using a bit of process management to ensure we have the optimal way of doing the book.”

From the chapter “Tumours of the stomach.” Intestinal-type adenoma. This adenoma is accompanied by intestinal metaplasia on the right side and shows prominent tumour-infiltrating lymphocytes; a subset of such adenomas are microsatellite-instable.
A key change in this edition is the classification of neuroendocrine neoplasms (NENs). “We had an expert group that met in November 2017 to solve some of the consistency problems that existed between the volumes in the classifications of NENs,” Dr. Cree says. “Within the digestive system, you obviously have quite a few different organs. We were able to ensure that the neuroendocrine neoplasms were dealt with similarly in each of those organs as a result. We also put soft tissue tumors and hematolymphoid tumors in separate chapters at the end. Having designated chapters let us treat the whole subject of those particular tumor types better.”
Some information issues, the editorial board found, have proved to be more difficult to address. Pathologists sometimes disagree on whether to change terms that are in day-to-day use, and there are certain more convoluted terms that the board would prefer to replace, Dr. Cree says. “We have certainly made changes to the names of tumors where we felt it was necessary, but we were aware there are multiple names in use across the world for some tumor types.” So, in many cases, “we have said what we feel is an acceptable terminology and what is not recommended for being outdated.”
The editorial board did agree to make changes in definitions in some terms relating to stomach cancer, but the process was not simple. “We try to achieve a consensus by having the expertise that we need in the room. You talk about the evidence and sometimes your decisions are fairly straightforward and sometimes they are not. If there is uncertainty, then what we now do is express that. If we don’t know what something is, we say that.”
Despite the value of the books in helping with diagnosis, Dr. Cree says, they can’t quite compensate for the small number of pathologists in the world and the increasing workload in histopathology, especially in high-income countries over the past 10 years. “We have the problem of how we handle the increasing complexity of what we’re being asked to do. Largely that is because it is no longer good enough to give a diagnosis. We hope the classification helps by making it clear what is required and what is not required and what the standards are.”
The classifications, he adds, are used by the International Collaboration on Cancer Reporting to produce synoptic reports; the CAP also uses the reporting templates. “Those templates help enormously to make sure patients get all the information they need from pathologists. I think that is extremely important today.” For the CAP cancer protocols as well, Dr. Washington says, “we will be looking at the new histology terms, and if there are any critical differences, they will be incorporated on the rolling update schedule. Minor differences will be incorporated but not until the next scheduled release of the protocols.”
WHO editorial board expert member David S. Klimstra, MD, chair of the Department of Pathology at Memorial Sloan Kettering Cancer Center and a professor of pathology and laboratory medicine at Weill Cornell Medicine, has been involved with the GI books and the endocrine organ books through three editions of the WHO series, spanning roughly 20 years. While the digestive system tumors include everything from the esophagus, stomach, intestines, colon, and liver to the pancreas and gallbladder, he worked most closely on pancreas, liver, and the neuroendocrine system.

Dr.Klimstra
The classification of liver tumors, especially bile duct tumors, has changed in this edition, he says, in ways that will affect patient treatment. “We made an effort to bring together a group of diverse tumor types that are now felt to fall under one broad category instead of several smaller categories, so that is an important change. Bile duct cancer classification has been condensed and simplified. Many variants have been collapsed into essentially two major categories of cholangiocarcinomas. This will make it a lot easier for pathologists to classify these kinds of liver cancer because the criteria to distinguish all previous variants were not well accepted.”
The classification of neuroendocrine tumors throughout the GI tract, which has been updated and standardized, is also significant, Dr. Klimstra explains. “We discovered over the past decade that simple classification into three grades that distinguish well-differentiated neuroendocrine tumors grades 1 and 2 from poorly differentiated neuroendocrine carcinoma grade 3 is actually wrong. In the current book, well-differentiated neuroendocrine tumors have three grades—G1, G2, and G3—that correlate with increasing proliferative rate and tumor aggressiveness. The poorly differentiated neuroendocrine carcinomas are a completely separate entity; they have a very poor prognosis and we aren’t even grading them anymore. This has allowed us to recognize a different spectrum of NENs than previously and to tailor the treatment to the specific genetic and pathologic subtype that the patient has. It applies to every organ in the GI tract, liver, and pancreas.”
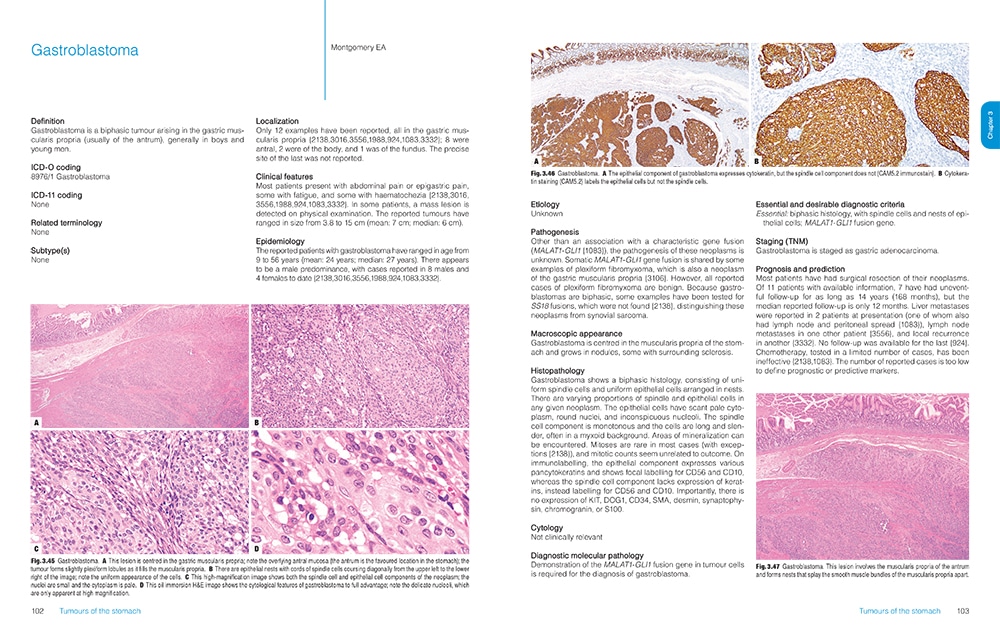

Sample pages from Digestive System Tumours, fifth edition. Each tumor type is described on the basis of its localization, clinical features, epidemiology, etiology, pathogenesis, histopathology, diagnostic molecular pathology, staging, prognosis and prediction, and, where appropriate, macroscopic appearance and cytology.
The WHO Blue Books are designed to be used by pathologists in an array of settings, Dr. Klimstra says. “Whether you are talking about a major academic center in the U.S. or Europe or a small hospital in a developing country, it’s intended to be used throughout the entire world.” Some countries have developed parallel classifications over the years and continue to reference them, but all pathology practices in the world are aware of the WHO Classification of Tumours Series and can access a printed copy or the online version.
Historically, the printed version of Digestive System Tumours has been a major reference produced once a decade, based on a series of meetings and input from experts who redraft the text and figures and illustrations. “Although it is technically not an atlas, in the sense of providing exhaustive illustration of every different variant of tumor that arises in every organ, it is well illustrated in the text version,” Dr. Klimstra says. “But when you are dealing with printed documents, it’s clunky. You can’t make minor updates when you need to achieve a consensus of experts.” So having the online version “will provide a simpler way for modifications to incorporate new data that will augment our understanding.”
Pathologists learn so much from their exposure to illustrations, he says, and high-quality graphics have always been a feature of the WHO Blue Books. “When you collect world experts together and they all have their archives of gross photographs and microscopic slides, you can produce the best examples and most classic illustrations of the features.”
Now, the incorporation of digital slides will allow an interactive experience for the reader, who will be able to look at not just a single snapshot, such as would appear in a book, but also different magnifications that can be examined more comprehensively. This capability has become practical only in the past few years, Dr. Klimstra says. The WHO has learned from the experience of PathPresenter, which has created an educational portal for digital slides that is now an entirely new feature of the WHO series.
The new descriptions of tumors by molecular phenotypes will be helpful in supporting diagnosis, he says. “Over the past decade, we have been doing a lot more molecular analysis of every cancer type and we understand there are certain key alterations, whether they are mutations, gene fusions, or other alterations, that are highly characteristic of certain tumor types. In some instances, the old classification system did not mesh perfectly with the new information we are getting from genomics.”
The editorial board’s decisions about which terms to recommend changing and which to leave alone, Dr. Klimstra says, were driven by several factors. “To some extent, how we name tumors is a matter of personal preference. Terminology can be fraught with various implications. Some people think the designations ‘tumor,’ ‘carcinoma,’ and ‘neoplasm’ all mean the same thing, but others say no, they have different implications. Over time, we’ve developed a lexicon that is in general usage and that most pathologists, and hopefully most treating physicians, understand.”
When you get a consensus group together, he adds, it’s natural to look at improving existing classifications. “The group may decide to make changes because of a subtle linguistic preference for one term over another. But the principle was that we shouldn’t make changes just because we can, but only because there is a rationale, hopefully based on data.” For example, “we realized that a variant of intraductal pancreatic neoplasm that had been regarded as related to a broader category of tumors is actually genetically different and should stand on its own as a separate entity. So that fed into the terminology change and classification change in this case.”
One challenge for the editorial team was how to clarify the often ambiguous lines between benign and malignant tumors. “There is ambiguity in certain circumstances where the pathologic findings don’t fully account for the malignant potential of a tumor,” Dr. Klimstra says. “For example, tumors of the appendix have been problematic for years because some look very benign and it is hard to predict if they will behave aggressively, but nonetheless patients develop abdominal dissemination from these appendix neoplasms.”
The editors chose a change in approach for a number of different neoplasm types to not strictly categorize things as benign or malignant. “We have the concept of a neoplasm of undetermined or uncertain malignant potential. That category persists because we simply don’t have rigid criteria for benign or malignant. Some of it has been resolved by talking about risk stratification. That is, we recognize a spectrum of biology from essentially benign on one end to fully malignant on the other end. Within this continuum, there are key pathology findings that can tell you how close you are to one end of the spectrum.”
Development of the WHO Blue Books is ongoing, says editorial board member Alexander J. Lazar, MD, PhD, professor of pathology and genomic medicine at the University of Texas MD Anderson Cancer Center. There are three books at various stages of editing and production at any one time under the direction of the standing editorial board and the 12- to 15-person boards of specific subject matter experts from around the world. Since the June publication of Digestive System Tumours, the breast tumor book became available online in August and was formally announced at the European Congress of Pathology in Nice, France. Writing is complete for the fifth edition of Tumours of Soft Tissue and Bone, which will be published next and followed by the gynecologic tumor and lung tumor books.

From the chapter “Tumours of the colon and rectum.” Traditional serrated adenoma (TSA). The cells lining the villi are predominantly tall and columnar, with abundant eosinophilic cytoplasm and centrally located oval nuclei with pseudostratification but no mitotic activity. Note the multiple ectopic crypt formations along the villi with differentiated goblet cells.
Dr. Lazar is enthusiastic about the online availability of the new books. “The website will be something we hope people will adopt and find as a good way to access this information as well. This website is very different from what was available previously, which was basically a giant PDF of the book. This was hundreds of pages, and while you could read it on a computer screen, it had no other type of functionality in terms of a user interface. The resolution was limited, and you were not able to magnify the photomicrographs significantly, have access to whole-slide images, or do complex word searching.”
The transition to online availability does, however, take the series into unknown territory, he says. “We are in the very early days for this, so what the uptake will be for the Web-based version versus print I don’t think we know yet. The number of books that are being printed and the rate at which the digestive book is selling are consistent with what we have experienced with the WHO books in the past.” In addition to the whole-slide images, the online version’s searchability will be much faster than consulting an index in a traditional book for every occurrence of a particular word or concept, he notes.
The price of the printed books—in the $130 to $150 range—is modest. The pricing model for the Web-based version of the books is still in flux, but Dr. Lazar expects it to be an annual individual user or site license fee to access all of the books that are online—which includes some books from the fourth edition and will eventually include all fifth-edition books as they appear over the next three to four years. The WHO pricing model takes into account the ability to pay in developed countries versus developing countries, and the Web platform will probably do so also, Dr. Lazar says.
The editorial board consensus on changing established, day-to-day terms in pathology was conservative: no change unless there was strong evidence and rationale for the change. But, Dr. Lazar says, a few such changes were made in the new edition. “The example that people notice the most is where part of the characterization of the tumor involves looking at counting mitoses per a particular defined area.”

Dr. Lazar
“A very common terminology used to characterize mitotic activity is a certain number of mitoses per high-power field. However, this terminology turns out to be quite imprecise because on different people’s microscopes, depending on how they are set up, a high-power field could mean very different things. In recognition of this, mitotic counts are given per defined amounts in an area—in most cases mitoses per millimeter squared—as opposed to using ‘10 high-power fields’ without a definition of what a high-power field is.”
Since the same tumor may be present across multiple organ systems, another priority was to make sure each book in the WHO series discussed the tumor in a way that is consistent with the other books. “A benign tumor such as schwannoma, for example, will characteristically involve multiple different organ systems and may be in as many as eight or more of the different books. Each book may describe slight differences in the way the tumor presents or looks in the different organ systems, but we want to make sure all the essential definitions are consistent with one another.”
The accelerated publishing schedule in this edition of the WHO series—with all books produced over six years from start to finish as opposed to over 10 years or more—is partly aimed at helping provide this consistency in definitions as well as in style and format, Dr. Lazar says. In addition, “we think the accelerated schedule is appropriate because our knowledge is expanding so rapidly; it is important to do interval updates frequently and efficiently.”
The WHO editorial board and expert panels walk a fine line in handling the wide range of technical sophistication of their worldwide readership, editorial board members agree. It’s a big challenge, Dr. Klimstra says. “You want to be applicable in all practice scenarios, but as molecular findings have been incorporated into cancer diagnosis, in practice settings without access to molecular findings you may not be able to apply classifications effectively. There’s an inevitable disconnect between highly technical practices, where there is enough sophistication and, frankly, monetary resources, versus others, where you have a microscope with stained slides and you have to do the best you can.”

From the chapter “Tumours of the gallbladder and extrahepatic bile ducts.” Tumour of the common bile duct. The small cell carcinoma component is seen in the cores of the papillae; it is positive for CAM5.2 in a dot pattern.
There may not be an elegant way to resolve this issue. “On the one hand, we don’t want a classification system that can’t be used by three quarters of the planet,” Dr. Klimstra says. “On the other hand, we cannot ignore the importance of data from novel technologies. The mutational analysis of KRAS and EGFR in lung cancer is standard care in industrialized countries but not readily available in the entire world. These are things in a global community we have to struggle with. But the WHO is trying to find the most effective classification with the least demand for highly sophisticated and esoteric testing.”
In the coming years, the question of how to incorporate molecular features into the basic classifications of tumors is likely to remain one of the most frequent topics of discussion by the WHO editorial board, Dr. Washington says. “Do we stick with the histology-based classification with an overlay from the molecular, or will it be more important to start with a molecular basis? That will be the big challenge.”
For now, the new Digestive System Tumours is an important milestone in pathology. “This book is the most up-to-date accumulation of knowledge about all of the different factors that go into classifying and predicting the outcome and the right treatment for cancers of the digestive system,” Dr. Klimstra says. “It has brought in expert knowledge from around the world and condensed in one place essentially everything you need to know to accurately diagnose this broad array of cancers. This has been a hallmark of the WHO classification for years, and it remains a vibrant part of how we understand the pathology of cancer. In that regard it is a singular effort in the world.”
Anne Paxton is a writer and attorney in Seattle. The WHO Classification of Tumours Online can be accessed at https://tumourclassification.iarc.who.int/welcome and includes the six most recent volumes from the fourth and fifth editions. For a limited time, the annual subscription fee of €160 is reduced to €100.