Charna Albert
February 2023—Traditional algorithm? Or reverse? Elitza Theel, PhD, D(ABMM), of Mayo Clinic, in an AACC session last year walked through the two primary diagnostic algorithms for syphilis, explaining where the complexities lie and how her laboratory uncovered inappropriate testing for neurosyphilis.
Syphilis cases are up in the past decade, and by 11 percent between 2018 and 2020 alone, said Dr. Theel, director of the infectious diseases serology laboratory at Mayo Clinic and Mayo Clinic Laboratories. In women, the increase is 30 percent, and more than 50 percent of all U.S. counties reported cases in women of reproductive age, according to a 2020 CDC report. The CDC reported an increase in congenital syphilis rates of 425 percent between 2012 and 2020, leading to a more than 600 percent increase in syphilis-related deaths in neonates and infants.
“Every time I think about that I get goosebumps because this is a preventable disease,” said Dr. Theel, who also co-directs the vector-borne pathogens service line and is a professor of laboratory medicine and pathology, Mayo Clinic. “It’s important given this rise in cases to make sure we are on top of our game when it comes to syphilis diagnostics.”
Syphilis cannot be cultured on routine media, Dr. Theel said. And molecular assays are not readily available and have limited sensitivity, depending on stage of infection and the specimen tested. “Histopathology is available and helpful in some situations but remains imperfect,” she said, because of the limited sensitivity and specificity of the stains. “So that leaves serology, and decades later we still rely on treponemal and non-treponemal assays to diagnose syphilis.”
The Food and Drug Administration has approved 13 automated and three manual treponemal assays, with the Treponema pallidum particle agglutination (TP-PA) assay considered the reference method. The non-treponemal assays are the rapid plasma reagin (RPR) and venereal disease research laboratory (VDRL) tests. “And we rely on a combination of these,” Dr. Theel said, referring to treponemal and non-treponemal assays, “because their performance characteristics are imperfect when used alone.”

Dr. Theel
The non-treponemal assays have low sensitivity in primary syphilis and in the latent and tertiary stages. VDRL sensitivity is 62.5 to 78.4 percent in primary syphilis and 64 percent in late latent disease, and RPR sensitivity is 62.5 to 76.1 percent in the primary stage and 61 percent in late latent disease (Tuddenham S, et al. Clin Infect Dis. 2020;71[suppl 1]:S21–S42). “The other important thing to remember is that RPR titers will decrease and decline even in the absence of treatment, but they will also decline during treatment,” she said. “So they’re used to monitor response to therapy, with most patients seroreverting to negative anywhere from 16 to 18 months after initiation of treatment.” About 30 percent of patients will remain seropositive at a low level, however, “and the clinical significance of that remains unclear.”
Dr. Theel is often asked if syphilis can be missed due to prozoning of the RPR. In one study of more than 2,000 cases of syphilis, she said, less than one percent of RPRs were falsely negative due to prozoning (Liu LL, et al. Clin Infect Dis. 2014;59[3]:384–389). “And in my 10 years as a lab director, I have yet to see us miss a case of syphilis due to RPR prozoning. So this is very rare. What’s not rare, though, are false-positive RPRs,” she said. False-positives are seen in less than two percent of samples, often in older individuals, and in those with recent vaccinations, in pregnant patients, in those with HIV, malaria, leprosy, and Yaws, as well as among patients with certain autoimmune diseases.
The treponemal assays have a significantly higher sensitivity in the primary and late latent stages, with the TP-PA at 86.2 to 100 percent sensitivity in primary syphilis and the enzyme immunoassays, chemiluminescence immunoassays, and multiplex flow immunoassays at 91.7 to 98.5 percent sensitivity in late latent disease, for example (Park IU, et al. Clin Infect Dis. 2020;71[suppl 1]:S13–S20; Loeffelholz MJ, et al. J Clin Microbiol. 2012;50[1]:2–6). “But they suffer from false-positives, primarily due to Epstein-Barr virus infections, Lyme disease, and select autoimmune diseases,” Dr. Theel said. And more than 90 percent of patients will remain seropositive for life, “so we can’t use treponemal assays to monitor response to therapy.”
The traditional diagnostic algorithm for syphilis begins with an RPR (Fig. 1). “If that’s nonreactive, that would suggest no evidence of syphilis,” she said, “but what we need to be thinking at this point is, could this be a false-negative due to primary or late latent syphilis?’’ If it’s reactive, “we’ve got to think, is this real or could this be a false-positive result?” The next step is a treponemal test. “If that’s nonreactive we would consider this an unlikely syphilis infection, with the RPR potentially a false-positive result. Whereas if we have two reactives, then you have a syphilitic patient and you’re done.”
The reverse algorithm begins with a treponemal immunoassay. “If it’s nonreactive, you can be fairly confident your patient does not have syphilis, unless exposure occurred super recently. But if it’s reactive, you’ve got to think, is this a recent infection, or could it be a past infection that has been treated, or is this a falsely reactive result?”
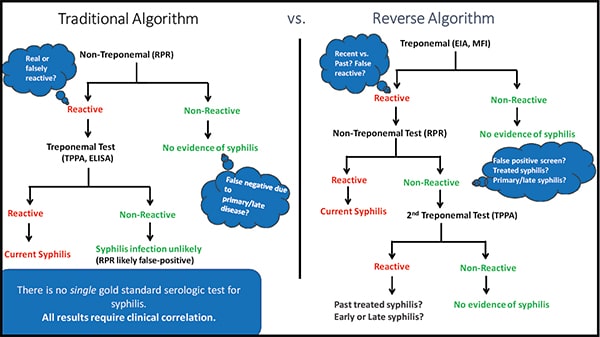
Fig. 1
The next step is an RPR. If the test is reactive, the patient can be diagnosed with syphilis. “The nonreactives get a little confusing, though, and this is where we have the most issues, from a clinician confusion perspective,” she said. A nonreactive RPR could mean that the treponemal screen was a false-positive, or that the patient had a past infection that was treated, or it could be a case of primary or late syphilis, when the RPR isn’t as sensitive. “To tease that apart, we do a second treponemal test,” she said, but using an assay that detects antibodies to antigens different from those targeted by the screening assay. Most often, the confirmatory treponemal assay is the TP-PA.
If the second treponemal test is nonreactive, the first can be considered a false-positive and the patient is clear. “But if it’s reactive, we’re still stuck,” she said. “And that’s where clinical correlation is needed, and it falls on the provider to get that more detailed history.”
“Bottom line,” she said, “there’s no single gold standard test for syphilis serology, and all results require that post discussion with clinicians.”
CAP checklist requirement IMM.41420 Anti-Treponemal Antibody Screening, revised in the 2022 checklist edition, says that if the laboratory used anti-treponemal antibody testing as a screening test for syphilis infection, all specimens with an initial positive result must have a non-treponemal test performed. If results of the two tests are discordant, a second treponemal test on a different platform (such as TP-PA) is required.
Which algorithm should a laboratory use? “The answer depends on the prevalence of syphilis in your institution, the cost of the testing you have available,” and test volume, Dr. Theel said. The traditional algorithm is better suited to smaller laboratories with a lower volume, in a non-highly endemic region. “Non-treponemal tests are cheap, they’re quick, and you don’t need to maintain automation.” For smaller labs serving a high-risk, highly endemic population, such as sexually transmitted disease clinics, the reverse algorithm is more appropriate. “And it’s also more appropriate for larger labs that have the ability to maintain automation.”
From a clinical perspective, the reverse algorithm is preferable because of its increased sensitivity in primary and latent disease compared with the traditional algorithm (95.83 percent in primary and 99.87 percent in late latent compared with 75 percent in primary and 73.07 percent in late latent, respectively) (Ortiz DA, et al. Clin Infect Dis. 2020;71[suppl 1]:S43–S51; Tong ML, et al. Clin Infect Dis. 2014;58[8]:1116–1124; Binnicker MJ, et al. J Clin Microbiol. 2011;49[4]:1313–1317). “But that comes at a cost, because up to about 17 percent [0.6–17 percent]—depending on which assay you use—of your treponemal-screened positive results ultimately will not confirm,” she said. The first test, then, would be positive, and the following two tests negative. “And that can lead to interpretive confusion. So when thinking about switching algorithms or making changes, for this reason alone it’s imperative that you make any decisions alongside your clinicians.”
Reporting can be a challenge because of the algorithms’ many steps, Dr. Theel said. “In my perfect world, we would be able to report all results simultaneously, rather than giving providers a step-by-step view of what’s happening,” she said, to avoid confusion. “Because our laboratory information system limits us and we can’t do that, we report the first screening result as reactive, rather than positive, and we indicate immediately that an RPR has been ordered” to help distinguish between infection with T. pallidum versus a falsely reactive treponemal antibody result. Under the result, they provide a direct link to the syphilis reverse algorithm, she said, “so our clinicians, if there’s any confusion, can click and follow along.” If the RPR is discordant from the screening assay, they indicate that reflexive testing for detection of T. pallidum-specific antibodies by the TP-PA assay has been ordered, and again provide the link to the algorithm.
Providing too many order configurations, or allowing physicians to step in at any point, will lead to inappropriate utilization, she said. “So we allow our Mayo Clinic providers to order only one of three things: the full algorithm for initial diagnosis; the RPR test only, which is to be used for response to therapy or diagnosis of congenital syphilis; or the VDRL test only, for assessment of potential neurosyphilis.” Despite that, she said, “we still see significant overutilization of our latter two standalone tests.” RPR testing should be performed once a month or once every few months when used to monitor response to therapy. “We saw a significant amount of serial testing within a seven-day period,” she said, so they added a soft stop alert in the LIS. “And that’s helped.”
VDRL testing, too, was being ordered in spinal fluid in patients without prior serologic testing for syphilis, “and that didn’t make sense,” she said. “So a couple years ago we decided to look at our VDRL test utilization.” She and her colleagues performed a 25-year retrospective review of all cerebrospinal fluid (CSF) VDRL test orders, as well as a chart review of all patients with positive CSF-VDRL results to look at final diagnoses (Sytsma TT, et al. J Gen Intern Med. 2021;36[1]:77–83). From January 1994 through February 2018, 33,933 CSF-VDRL tests were performed on 32,626 patients. “Of all that testing, we had only 60 positive samples on 50 patients,” a positivity rate of 0.18 percent. “Everything else was negative,” she said.
In the chart review, of the 60 positive samples, 43 samples from 35 patients were found to be true positives. “They truly had neuroinvasive syphilis,” Dr. Theel said. The other 17 were false-positives, from 15 individual patients. All 35 of the patients with positive results were seropositive, meaning they had prior positive syphilis serologic test results. None of the patients with false-positive CSF-VDRL results had prior positive treponemal or non-treponemal antibody test results in serum, “and 60 percent of them ultimately were diagnosed with a central nervous system malignancy,” she said.
Dr. Theel and coauthors also looked at whether a subset of 8,553 patients with CSF-VDRL-negative results had prior syphilis serologic testing. Of the 8,553 patients, a third (2,855) had prior negative syphilis serologic test results, and 64.8 percent (5,543) did not have any prior syphilis serologic testing performed. One hundred fifty-five patients (1.8 percent) had at least one positive or equivocal syphilis serologic blood test result. “So only about two percent of our 8,553 patients had VDRL testing that was in some way indicated. This was concerning,” Dr. Theel said. Her plan is to establish a rule requiring that patients have a positive syphilis serology result “before VDRL testing is even considered to be ordered.”
Charna Albert is CAP TODAY associate contributing editor.