Karen Lusky
July 2017—Kisha Mitchell Richards, MBBS, a pathologist at Greenwich Hospital, Yale New Haven Health, Greenwich, Conn., recalls that when she was a resident, adenoma was just adenoma. “Nowadays it’s not quite where breast is, where it’s a two-page report, but there are now subtypes of hepatocellular adenomas,” she said in a CAP16 presentation on liver neoplasms. The subtypes are the HNF1 alpha or TCF1 inactivated adenoma, inflammatory adenoma, beta-catenin mutated adenoma, and the unclassified adenoma, which she notes is basically adenoma NOS (not otherwise specified).
The HNF1 alpha or TCF1 inactivated adenoma is frequently but not always steatotic. “So certainly if you have diffuse steatosis, you think of that subtype,” Dr. Richards said. “It’s commonly associated clinically with young women with or without diabetes. The immunostain used for that is a liver fatty-acid-binding protein, and you usually have a loss of expression in those.”
If you see an adenoma and wonder if it’s focal nodular hyperplasia, she said, it could be an inflammatory adenoma. “The adenoma looks inflammatory and there’s often sinusoidal dilatation.” Focal nodular hyperplasia can look inflammatory, she told CAP TODAY in an interview. “That’s why it can be confused with the inflammatory adenoma. Often an FNH has inflammatory cells.”
Dr. Richards cautioned that some of the inflammatory adenomas have the beta-catenin mutation and are at risk for progressing to hepatocellular carcinoma. The stains that tend to be used for the inflammatory adenoma are serum amyloid A and C-reactive protein, she said, adding that she usually uses the former. (The amyloid stain may also be positive in an inflamed liver.)
“If [the lesion] is benign appearing, you see some fibrous bands and central scar, ductular proliferation and inflammation, and you think it’s an FNH, use glutamine synthetase and amyloid A, depending on the setting, to help distinguish the inflammatory type [of adenoma] versus an FNH,” Dr. Richards advised.
Glutamine synthetase is useful in FNH, she says, because it has a different pattern of staining in FNH, “a geographic pattern of staining.” However, “you can also have what is called pseudo map-like positivity,” she cautioned. She discussed a study by Nancy Joseph, MD, PhD, and Sanjay Kakar, MD, of the Department of Anatomic Pathology, University of California, San Francisco, and colleagues that addresses that subject (Joseph NM, et al. Mod Pathol. 2014;27[1]:62–72). In their article, the authors wrote, “The majority of inflammatory hepatocellular adenomas demonstrated perivascular and/or patchy glutamine synthetase staining (73.6%), while the remaining cases had diffuse (7.5%), negative (3.8%), or patchy pattern of staining (15%) that showed subtle differences from the classic map-like staining pattern and was designated as pseudo map-like staining.” The “pattern was observed focally at the periphery of the lesion,” they noted.
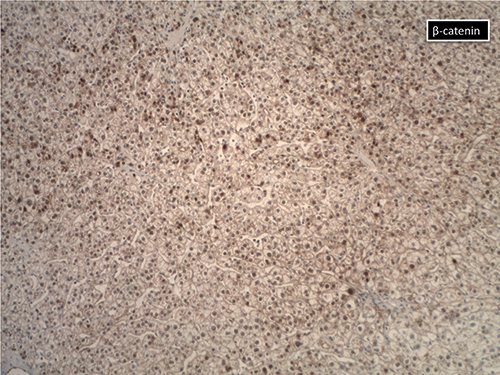
Courtesy of Kisha Mitchell Richards, MBBS
If an adenoma looks atypical, Dr. Richards said, it could be a beta-catenin mutated subtype. “Some American pathologists think that some of these lesions are actually already well-differentiated HCCs,” she says. “The difficulty comes when you try to use the beta-catenin stain [below] because it can be very, very focal” and can appear to be negative. Some pathologists have used strong glutamine synthetase overexpression as a surrogate. “There is always the risk in a biopsy,” however, Dr. Richards cautions, “that what appears to be diffuse overexpression is just oversampling of one area of a tumor that is more heterogeneous than represented on the biopsy.”
There’s another caveat. Although strong diffuse glutamine synthetase positivity can indicate presence of a beta-catenin mutation, Dr. Kakar and colleagues have conducted studies showing this is not always true, Dr. Richards said. “It can be, so certainly if you are confronted with that type of pattern, it’s something you need to report, to say this may suggest that it harbors a beta-catenin mutation.”
In an interview with CAP TODAY, Dr. Kakar, UCSF professor and chief of GI-hepatobiliary pathology services, said that based on studies conducted in France, “diffuse GS staining is thought to have high correlation with beta-catenin activation.” He notes, however, that a study he and colleagues reported last year showed that the CTNNB1 exon 3 mutations, the gene that encodes beta-catenin, are present in a subset of cases but not every case that has diffuse GS staining (Hale G, et al. Mod Pathol. 2016;29[11]:1370–1380).
In that article, Dr. Kakar and colleagues wrote: “Of hepatocellular tumors with diffuse glutamine synthetase staining (homogeneous or heterogeneous), an exon 3 β-catenin mutation was detected in 33% (2/6) of typical hepatocellular adenoma, 75% (3/4) of atypical hepatocellular neoplasm and 17% (8/47) of hepatocellular carcinomas.” An exon 3 mutation was also observed in 15 percent (2/13) of HCCs with patchy GS staining. The correlation was low in this study partly because of the use of paraffin-embedded tissue, Dr. Kakar says, and the true discrepant rate between diffuse GS and absence of underlying genetic changes to account for it is perhaps about 25 percent.
The researchers defined diffuse homogeneous GS staining as “moderate-to-strong cytoplasmic staining in >90% of lesional cells, without a map-like pattern.” Diffuse heterogeneous was moderate-to-strong staining in 50 to 90 percent of such cells with no map-like pattern of staining.
“It is quite likely,” Dr. Kakar tells CAP TODAY, “that diffuse homogeneous GS staining correlates more strongly with beta-catenin activation, while diffuse heterogeneous staining has a less strong correlation.” The type of underlying mutation influences the pattern of staining, he adds, “with D32-S37 deletions/mutations and T41 mutation leading to a diffuse homogeneous pattern, while S45 mutation leads to relatively weaker beta-catenin activation resulting in a diffuse heterogeneous pattern”(Rebouissou S, et al. Hepatology. 2016;64[6]:2047–2061). “Mutations in the exons 7 and 8 of the CTNNB1 gene can also occur, leading to weak beta-catenin activation and patchy GS staining in most cases,” he says.
“The correlation between type of mutation and GS staining pattern was reported to be nearly 100 percent” in the study by Rebouissou, et al., he reports. But the correlation isn’t perfect, “and several exceptions were noted in our Modern Pathology 2016 study.”
Dr. Kakar thus concludes that “the specificity of diffuse GS staining—especially diffuse heterogeneous—is not perfect for the high-risk CTNNB1 exon 3 mutation, and molecular assays may be necessary for appropriate risk stratification in these cases.” Molecular assays may also be helpful in cases where GS staining pattern is equivocal, he adds. “On the other hand, the sensitivity of diffuse homogeneous GS staining is high, and it is unlikely to have a high-risk CTNNB1 exon 3 mutation without diffuse GS staining, although rare exceptions to this were noted in HCC in our Modern Pathology 2016 study.”
A combination of molecular assays is likely to be required for risk assessment in the setting of well-differentiated hepatocellular neoplasms in selected clinical settings (e.g. tumor
“Whether a well-differentiated hepatocellular neoplasm with beta-catenin activation is an adenoma or HCC is a complicated topic,” Dr. Kakar says. “If there are obvious atypical morphologic features or reticulin loss, the diagnosis of HCC is straightforward.”
Dr. Kakar points out that the 2010 World Health Organization classification categorizes tumors that have beta-catenin activation and no atypical features as beta-catenin-activated adenoma. However, “there is no definite category for tumors with borderline atypical features,” he says. They showed in the 2013 Human Pathology study that most beta-catenin-activated tumors can be classified as HCC based on careful review of morphology and reticulin stain, while the remaining should be categorized as atypical hepatocellular neoplasms. In response, he says, “a group of international liver pathology experts proposed the term ‘hepatocellular neoplasm with uncertain malignant potential’ (HUMP) for these borderline tumors” (Bedossa P, et al. Hum Pathol. 2014;45[3]:658–660).
“It is my hope,” Dr. Kakar says, “that the new WHO classification will take these findings into account and create a separate category of atypical neoplasms that lack obvious diagnostic features of HCC but have high-risk features such as beta-catenin activation.” He is not aware of any scheduled date for the new classification.
Dr. Richards told CAP16 attendees that it is important to remember that if they are looking at an adenoma and wondering if it’s a well-differentiated HCC, then it could be one of these subtypes. “And especially in a man, you want to be very careful about calling it just adenoma,” she said. “You may want to then call it an atypical hepatocellular proliferation and raise that differential.”
[hr]
Karen Lusky is a writer in Brentwood, Tenn.