Karen Lusky
March 2017—Keep eyes wide open to everything and describe everything because there might be a number of different factors playing into a patient’s disease. That was the reminder Robert M. Najarian, MD, opened with last fall in his CAP16 presentation on common patterns of liver injury.
Dr. Najarian, a consultant in gastrointestinal, hepatobiliary, and pancreatic pathology at Beth Israel Deaconess Medical Center and Harvard Medical School, began with a case to illustrate.
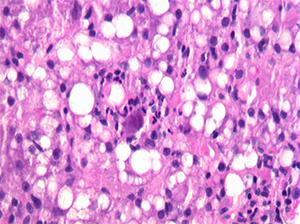
Fig. 1
A hepatologist wanted to know if a jaundiced patient was still imbibing alcohol. The patient had a history of past alcohol abuse and was transplanted for alcoholic steatohepatitis. In an image he showed of the biopsy of the woman’s transplanted liver (Fig. 1), Dr. Najarian noted there was clearly an active steatohepatitis present. But then he described a feature visible in the center of the image: “This very large sort of smudgy-looking cell with some eosinophilic—what look like—inclusions.”
The biopsy really had two stories to tell, Dr. Najarian said. One was alcohol use. The patient had not been following up with her physicians but returned for care after her skin became yellow after heavy drinking at home. And she had cytomegalovirus infection, commonly seen in post-transplant patients.
“The whole purpose of showing that case to everyone was to highlight that we sometimes focus on the most obvious histologic finding and run with it and blame the patient’s presentation on a single entity,” Dr. Najarian tells CAP TODAY.
In his presentation, Dr. Najarian reviewed the common patterns of liver injury seen in medical liver biopsies, including the steatohepatitic or toxic-metabolic pattern, commonly associated with alcohol, excessive weight and other metabolic syndrome risk factors, and other inherited and acquired metabolic diseases. Some patterns are specific for particular disease entities. “These usually fall into the realm of certain viruses that you can clearly identify on H&E-stained slides,” he said. Other common patterns are a biliary or cholestatic pattern, with bile duct obstruction as the “classic example,” a vascular pattern of injury, and an active or chronic hepatitic pattern. The latter is frequently associated with, among other things, autoimmune hepatitis and viral hepatitides.
Dr. Najarian focused on what he called the “dreaded visitors” that pathologists don’t want to see on their microscope stage: eosinophils, plasma cells, and steatotic hepatocytes in liver biopsies. “When we see eosinophils, we wonder how specific is this for any one particular entity,” he said. “Am I dealing with a drug reaction, which, after all, is supposed to have eosinophils? Am I dealing with a parasitic infection, which would be very unusual? Or is this just something else where the eosinophils are coming along for the ride?” Where, he asked, can the pathologist find clarity?
Are pathologists always dealing with an autoimmune hepatitis or an immune-mediated type of injury when they see plasma cells? “And what other laboratory data or information should I be looking for to help provide clarity in this instance?”
Cases in which steatosis is a concern are less of an issue in terms of identifying them because it’s fairly easy to see, he said. More important, in his view, are specificity and knowing what questions to ask the clinician and the patient.
Dr. Najarian presented case studies and other material on each of the microscopic visitors, starting with eosinophils. He described the first example as “a strange case of eosinophils causing havoc.” It was “an extremely uncommon pattern,” Dr. Najarian tells CAP TODAY, unlike anything he’d ever seen before.
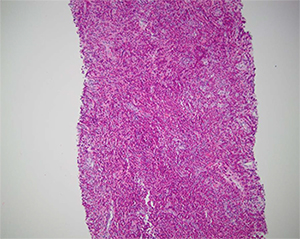
Fig. 2
The clinician was suspicious that a 54-year-old male patient had a neoplastic process. The patient had multiple mass-forming lesions in the liver but no history of a previous cancer. Dr. Najarian believed at the outset that it was a tumor of unknown origin and thought, “Let’s get the immunostains ready for that purpose.” The patient had a 100-pack per year smoking history, hypertension, and hyperlipidemia. He had no recent foreign travel or history of infection, sick contacts, or unusual food consumption.
However, when Dr. Najarian initially looked at the biopsy under the microscope, he was taken aback. “It was actually the most splendid example of eosinophilia in the liver I have ever seen. And I said, ‘My God, there’s nothing but the eosinophils here,’” he recounted in his talk, showing an image of the biopsy. There weren’t any neoplastic cells except potentially neoplastic eosinophils, but all of the eosinophils were of normal morphology (Fig. 2).
Dr. Najarian said that he ultimately looked in other fields and observed a background of pale staining cells that had amphophilic cytoplasm and spindle-shaped nuclei, which he showed in a separate image. He didn’t see any parasite eggs, microorganisms, or indication of an organizing abscess. “Certainly, eosinophils made me think of ruling out infection,” he said, “but generally when [there’s] an infection and a consequential abscess, you typically expect to see some neutrophils, or in the organizing phase, you’d see some form of granulation tissue and not really one isolated cell population, the eosinophils, standing out. They tended to be in the background of other cases I had seen” (Fig. 3).
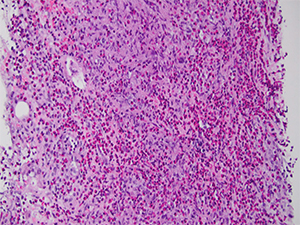
Fig. 3
Dr. Najarian said he did a mast cell tryptase stain, thinking, “Could those spindle cells be mast cells because we know they can look like anything, and anywhere there are mast cells there are commonly eosinophils because of a common group of cytokines that recruits them.” His short list of possible differential diagnoses included a mast cell neoplasm or a reactive proliferation of mast cells in the setting of a hematologic disorder consisting primarily of eosinophils. But the mast cell tryptase was negative.
The spindle cells were S-100 positive, however, which he said caused him briefly to ask whether the patient had a “bizarre sort of melanoma.” “[S-100 is positive] basically in all cells derived from neural crest origin, which includes melanocytes and other cells derived from the peripheral nervous system,” he says. So how did he rule out melanoma? “The fact that the eosinophils were the predominant population and the spindle cells only made up a very small population was one clue on the H&E-stained slides alone, but then also the positivity of those spindle cells for CD1a,” he says. “The co-expression of CD1a and S-100 would exclude melanocytes as the cause of that because melanocytes are CD1a negative.”
Dr. Najarian also contemplated other causes like a parasitic infection, he says, “because eosinophils are oftentimes increased within the tissue in response to local parasitic infection.” But the diagnosis was Langerhans cell histocytosis, “proven by immunoreactivity of the focally prominent spindle cells for CD1a and S-100.” Extra-pulmonary multisystem involvement, usually of the lymph nodes, liver, bone, and other sites, is more common in kids but not unheard of in adults, he says. Interestingly, “squashed in the bottom” of the CT chest evaluation was a note that the patient had many lung nodules described as “ground glass change, probably infectious,” Dr. Najarian told attendees. A subsequent biopsy of one of the nodules showed the same process observed in the liver.
“The pathogenesis of Langerhans cell histocytosis is still kind of a mystery,” he says, though the patients are treated with cytotoxic chemotherapeutic agents. What probably excludes it from being considered by all as a malignancy, he adds, “are spontaneous remissions that can occur in some patients without such treatment, however.”
[hr]
The optimal pre-biopsy laboratory workup
Dr. Robert Najarian says that his institution, Beth Israel Deaconess Medical Center, has a wonderful group of hepatologists who know what constitutes an optimal laboratory workup before a patient moves on to biopsy. But for pathologists who don’t have liver specialists at their hospitals, Dr. Najarian says he would argue that there are minimum requirements in terms of laboratory testing that he’d want to review before making a differential diagnosis and reaching conclusions about a patient’s biopsy. In addition to a basic metabolic panel, the tests include:
- Liver function tests that evaluate acute hepatocellular function (ALT and AST), and markers of bile duct injury (alkaline phosphatase, GGT, and bilirubin).
- Coagulation parameters, platelet count, and albumin to assess the patient’s synthetic function for possible chronic liver disease.
- Viral serologies (HBV, HCV, and others), in addition to autoantibody serologies (antinuclear, anti-smooth muscle, antimitochondrial antibodies, among others) to diagnose specific liver diseases.
Dr. Najarian says iron studies are important, too, including genetic testing for hereditary hemochromatosis in at-risk individuals or those with abnormal iron parameters. “If we are talking about younger patients with chronic liver disease and cirrhosis, studies for copper should be performed as well,” he says. “We know that Wilson’s disease is a cause or contributing factor to liver disease, especially in young patients, that may make them more susceptible to certain exposures to drugs and alcohol.”—Karen Lusky
[hr]
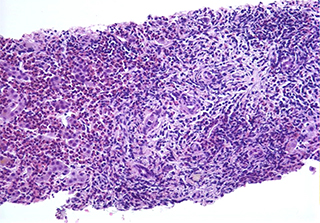
Fig. 4
In a second case involving eosinophils, a 43-year-old male had a history of a seizure disorder previously treated with carbamazepine. He had recently started taking another anticonvulsant, lamotrigine, and then developed jaundice, weakness, and fatigue. “No foreign travel, sick contacts, or unusual food consumption, and here we go again,” Dr. Najarian said.
When questioned further, the patient denied having a fever but reported that he had a prolonged rash that wasn’t in a contact dermatitis type of distribution. An H&E slide of the patient’s liver biopsy viewed at high magnification revealed “an immunoallergic hepatitis showing a chronic active portal-based hepatitis with eosinophils comprising the majority of the inflammatory cell infiltrate,” Dr. Najarian says (Fig. 4).
At first the patient didn’t have peripheral blood eosinophilia but later developed it, which Dr. Najarian noted can be defined in absolute or relative terms. Patients with immunoallergic hepatitis can also pre-sent with atypical lymphocytosis, he said. “Facial edema with adenopathy or arthralgias can also accompany this pattern of hepatitis.”
“This particular entity is defined by a clinical course which can occur in as few as eight days after exposure to the offending agent but can also take up to eight weeks to develop,” Dr. Najarian explained. The patient in this case took a couple of weeks to get to presentation. “Causes are largely due to antibiotics but also certain classes of anticonvulsants, HIV medications, and allopurinol.” If the clinician takes the patient off the drug and restarts it later, transaminitis will occur quickly, he warned.
Dr. Najarian reminded CAP16 attendees that the three components of the “diagnostic triad” for acute cellular rejection in an allograft liver biopsy include “a portal mixed infiltrate that can commonly have prominent eosinophils.” However, the eosinophils are not specific to rejection. The findings more specific to rejection are lymphocytic bile duct damage in addition to venous subendothelial inflammation, which usually affects the portal tracts first, though a certain percentage of patients may display central venulitis initially, Dr. Najarian said.
At least two of three of the components are required for an acute cellular rejection diagnosis, but only subendothelial inflammation is relatively specific for the diagnosis.
[hr]
Seeking optimal samples
In medical liver pathology, “Tissue is not the only issue but it is a big issue in allowing us to do the best job that we can,” says Dr. Robert Najarian of Beth Israel Deaconess Medical Center and Harvard Medical School.
“Ideally, you should be looking for something in the neighborhood of a 1.5 to 2.0 centimeter in length fragment of tissue,” Dr. Najarian said in his CAP16 presentation. That doesn’t mean “an aggregate of smaller bits,” he said, but intact fragments of 1.5 to 2.0 centimeters in the greatest dimension that optimally contain between eight and 12 portal tracts.
Pathologists can receive any number of various types of biopsies, which are most often percutaneous ultrasound or CT-guided biopsies, he said. But they can also get transjugular- or transvenous-obtained specimens, which he said “provide significant limitations with respect to size.”
The “new kid on the block,” Dr. Najarian said, is the endoscopic ultrasound-guided liver biopsy. At Beth Israel Deaconess Medical Center, they “happen to be very good samples and totally akin to the percutaneous samples,” he said. In other places where there is less experience with EUS-guided procedures, “you may be dealing with the same issues as you might have with the transvenous or transjugular biopsies.”
Surgical wedge biopsies—especially those performed for purposes of determining the stage of fibrosis or if the patient is cirrhotic—“are fraught with all sorts of issues,” Dr. Najarian cautioned, “because we know the liver has a very dense fibrous capsule, which can result in over-staging of fibrosis.” Additionally, intraoperative frozen section evaluation can introduce artifacts that can have an impact on fibrosis stage and ability to diagnose steatosis and inflammation accurately. Therefore, he recommends that a needle core biopsy be done intraoperatively, if possible, with standard histopathologic assessment (permanent sections) after surgery.
Dr. Najarian said that at his institution, which may differ from other practices, pathologists routinely get multiple H&E-stained slides, a Masson’s trichrome stain, and an iron stain. Then they order additional stains as the cases require. “Masson’s trichrome stain assesses the amount of fibrosis, which is a marker of chronic liver injury,” he says. “Depending on the pattern of fibrosis, we can determine whether a patient is cirrhotic, but also can make educated guesses about what the cause of the patient’s injury was.” (The trichrome stain can’t be performed intraoperatively.)
What can pathologists do to help ensure tissue isn’t the issue? Dr. Najarian says he sees an opportunity for pathologists to work not only as quality assurance agents with the physicians who perform these interventional procedures to obtain liver biopsies, “but also to challenge the marketplace, the makers of medical devices which obtain biopsy tissue, to develop devices that will provide optimal samples for us to make diagnoses.”
“Honestly, in a lot of cases,” he says, “pathologists are making diagnoses with big consequences and trying to do so with less tissue. It doesn’t have to be that way.”—Karen Lusky
[hr]
Dr. Najarian next addressed plasma cells. “Anytime prominent plasma cells are seen, the thought is that the body is mounting a heightened immune response with an increased production of immunoglobulins,” he says. This can be seen in post-transplant hepatitis, autoimmune hepatitis, or acute viral hepatitis.
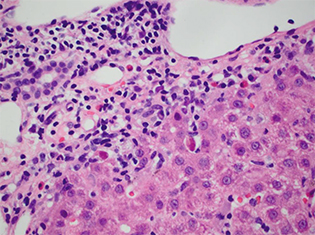
Fig. 5
In a case in which “plasma cells were on the scene,” a 36-year-old previously healthy-seeming male presented acutely with jaundice, abdominal pain, and fatigue. His ALT and AST exceeded 1,000, so he had a severe hepatocellular injury. The total bilirubin was greater than 15. The patient’s platelets and albumin were normal, however, “speaking to normal synthetic function—so no chronic liver disease by lab results anyway,” Dr. Najarian reported. “The common hepatitis serologies are negative and, significantly, the ANA titer is 1:1280.” The patient had taken topirimate on an as-needed basis for migraine headaches but had not done so for six months.
At high magnification, the patient’s biopsy showed “a portal-based hepatitis with prominent plasma cells and apoptotic hepatocytes at the interface, diagnostic of typical autoimmune hepatitis,” Dr. Najarian says. “Additionally, within lobular parenchyma, prominent plasma cells are seen to create rosettes around individual hepatocytes that demonstrate swelling with increasing injury, diagnostic of a typical active autoimmune hepatitis” (Fig. 5).
The official diagnostic criteria for autoimmune hepatitis set forth by the American Association for the Study of Liver Diseases take into account laboratory factors way before they consider the biopsy, Dr. Najarian said. These criteria are as follows:
- Serum biochemistry tests, which are abnormal ALT and AST. “They don’t really specify how much until you deal with more detailed scoring systems,” he noted.
- Serum immunoglobulins. “IgG is oftentimes markedly above the upper limit of normal, and in this case 1.5 times,” he said.
- Serum autoantibodies. That’s “antinuclear antibodies as a screening test but also the more specific autoantibodies: anti-smooth muscle, liver kidney microsomal, and soluble liver antigen antibody.”
- Negative viral serologies (HAV, HBV, HCV). “We know that viral hepatitis, especially in the acute form, can have prominent plasma cell infiltrates,” he said. “So we want to exclude those as the causes” and other contributing factors such as drugs or alcohol.
Fig. 6
Dr. Najarian said that if hepatologists use AIH scoring systems to support biopsy findings, he urges pathologists to at least familiarize themselves with the simplified version that he showed in his talk (Fig. 6), noting that it’s been found to be almost as good as a much more complex one, which he also shared with CAP16 attendees. In the abbreviated version, liver histology is given two points for “typical AIH,” and one for “compatible with AIH.” Often patients won’t have the “classic plasma-cell-rich lobular infiltrate rosette patterns” seen in typical AIH, Dr. Najarian cautioned. “So any hepatitis that seems to be portal-based, that has the interface hepatitis, mixed inflammation, could be compatible with AIH”—and that’s the score of one. He defines interface hepatitis as “hepatocyte apoptosis at the parenchymal interface with portal tracts.”
A subset of patients with primary biliary cirrhosis (PBC), which typically doesn’t respond to initial treatment with urodeoxycholic acid, may have a PBC overlap syndrome with autoimmune hepatitis, he says. Thus, Dr. Najarian notes that he always encourages pathologists to look at the patient’s ALT and AST to see if the patient has significant hepatocellular damage as well as damage to bile ducts before looking at the biopsy. To detect bile duct damage, pathologists should primarily look at alkaline phosphatase, he advises. “Generally [patients with PBC] have markedly elevated alkaline phosphatase,” he said, “and antimitochondrial antibodies are seen in about 90 to 95 percent of patients with PBC. So it’s a very sensitive and specific marker as far as autoimmune markers go.”
“If the patient has PBC that’s resistant to therapy, they are typically biopsied before they are placed on a steroid course,” he said. “Why? Simply because pathologists won’t see the autoimmune hepatitis component unless the patient is off of steroids.” He notes that the AIH component of injury is extremely sensitive to treatment with steroids and other immunomodulators.
“A patient’s biopsy with AIH/PBC overlap syndrome would typically exhibit significant lobular inflammation, often composed of prominent lobular plasma cells, with hepatocyte apoptosis, in addition to the lymphocytic bile duct injury,” says Dr. Najarian, noting that the bile duct injury is the most sensitive feature for a PBC diagnosis. “Additionally [in PBC], one can see significant portal lympho-plasmacytic inflammation, sometimes with a granulomatous reaction around a damaged bile duct [called a] florid duct lesion.” Dr. Najarian sometimes uses a cytokeratin 19 stain to identify markedly damaged bile ducts.
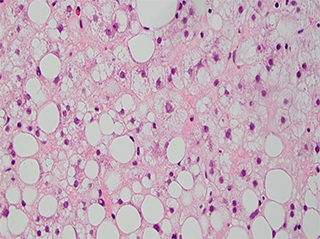
Fig. 7
Turning his attention to steatotic hepatocytes, Dr. Najarian noted that the central features of both alcoholic and nonalcoholic steatohepatitis are steatosis, ballooning degeneration of hepatocytes, and lobular mixed inflammation, with or without intracytoplasmic hyalin. “When you see hyalin prominently, you worry. You think more about alcohol,” he said. Sometimes in cases of florid acute alcoholic steatohepatitis, he says, cholestasis is also seen, which can help differentiate it from nonalcoholic fatty liver disease causes.
Dr. Najarian showed an H&E-stained example of steatohepatitis that had macrovesicular (large droplet) and microvesicular (small droplet) steatosis. He described the former as a phenomenon in which “a hepatocyte nucleus pushed off to the side of the cell” and the latter as “multiple fat droplets within a single hepatocyte.” In addition, “enlarged hepatocytes with preserved nuclei and a ragged, intracytoplasmic appearance typical of ballooning degeneration are seen,” he says (Fig. 7).
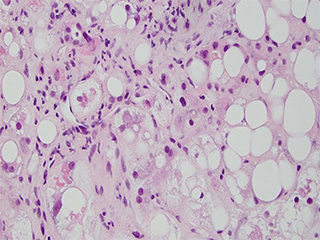
Fig. 8
Dr. Najarian shared a case in which he says a diagnosis of fatty liver disease was a surprise. A 74-year-old female patient presented with abnormal liver function test results. She reportedly stopped drinking alcohol more than 15 years previously and didn’t drink heavily even then. Viral, autoimmune, and metabolic test results were normal. With a BMI of 20, she was “on the underweight side,” he said. She had diagnoses of atrial fibrillation and hypertension but no diabetes or hyperlipidemia.
At high magnification, an H&E-stained image of the patient’s biopsy demonstrated “prominent ballooning degeneration of hepatocytes with ropey, intracytoplasmic hyalin and scattered neutrophils mimicking the typical histologic appearance of alcoholic steatohepatitis,” he says (Fig. 8).
Seeing this “spectrum of findings,” you begin to be tempted to say the patient isn’t telling the truth and is drinking every night, Dr. Najarian said. And in some instances, patients don’t tell the truth and their hepatologists will report that they don’t trust the history, which is important for the pathologist to be aware of. But in this case, the clinician had no reason not to believe the patient.
“So what could be going on here?” he asked. “Because for all intents and purposes this is steatohepatitis in a patient who is not overweight and not drinking.” The patient had been taking an antiarrhythmic agent, amiodarone, for eight months until she was discovered to have abnormal liver function tests. And amiodarone is a “classic example of a drug with a very specific pattern of injury: that which mimics alcoholic steatohepatitis in all its forms, hyalin included—very prominent hyalin.”
Tamoxifen, steroids, and chemotherapeutic drugs like cisplatin and irinotecan can also cause fatty liver disease, although it won’t necessarily be so much “an alcoholic picture,” Dr. Najarian said. “You should also exclude other causes like Wilson’s disease, which is actually a common cause of fat in the liver, rare metabolic disorders like tyrosinemia, and, of course, alcohol or even starvation, for a depleted nutritional state can also present with abnormal LFTs and fatty liver pattern of injury.”
Fig. 9
Pathologists are sometimes asked when patients with past histories of alcoholic steatohepatitis have last consumed alcohol, Dr. Najarian noted. While not always the case, hyalin and ballooning degeneration often require a long time to resolve, he said, displaying, in contrast, the image of a biopsy from someone who hadn’t abstained for long. The specimen had prominent ballooning degeneration, neutrophils, and intracytoplasmic hyalin. By contrast, a biopsy from the same patient after being abstinent for several months showed that the ballooning hadn’t gone away and certainly not the hyalin, he said. The fat had resolved, as well as the neutrophils to some extent, “but remember that neutrophils won’t entirely go away because hyalin is a chemoattractant and will by nature attract neutrophils.”
Dr. Najarian said that even though quantitative scoring systems such as the NASH Activity score were designed to evaluate patients whose liver injury isn’t due to alcohol, he “algorithmically” uses it for all patients who have fatty liver disease or steatohepatitis just so the hepatologist can know what he found on the biopsy (Fig. 9).
Dr. Najarian concluded his talk with “pearls of pathology” about the “dreaded visitors.”
“Eosinophils often are a component of many diverse causes of liver injury, not just drugs or allergy,” he said. “Plasma cells aren’t specific for autoimmune hepatitis but are frequent contributors to diseases [and drugs] where there is an immune-mediated injury.” As for fatty liver disease, “History is really everything in this particular case,” he said, “and excluding specific common causes” is very important.
[hr]
Karen Lusky is a writer in Brentwood, Tenn. All images are courtesy of Robert M. Najarian, MD.