Amy Carpenter Aquino
March 2022—Recent years have seen new releases in allergy and autoimmune disease testing that move the fields forward.
“On average we’re looking at six to 10 years of a patient going through the process of seeing specialist after specialist and finally reaching a diagnosis,” Veena Joy, MSc, PhD, Thermo Fisher clinical affairs manager of autoimmunity-immunodiagnostics, says of autoimmune disease. “Autoimmune diseases have low incidence and prevalence rates, so the specificity of the assay is critical.”

Joy
Thermo Fisher’s EliA SmDP-S assay to aid in the diagnosis of systemic lupus erythematosus, cleared by the FDA last year, was designed and developed to enhance specificity without compromising the sensitivity, Joy says. “We revamped our existing EliA SmDP assay to have increased specificity,” which helps physicians differentiate lupus from mixed connective tissue disease, “providing a higher degree of diagnostic confidence.”
The SmD3 peptide has been identified as the most specific Sm antigen for SLE. The EliA SmDP-S, Joy says, combines a synthetic version of this SLE-specific SmD3 peptide with an advanced coating technique that optimizes the binding of the SmD3 peptide antigen, “further improving specificity and therefore supporting a more precise diagnosis.”
Werfen’s next-generation Aptiva system was also cleared last year, with the first U.S. implementation to get underway soon, says Bill Manchester, vice president of worldwide marketing and service for Werfen Autoimmunity.
With the new system, he says, Werfen is combining biomarkers to address a disease state. For connective tissue disease, for example, “we can have an essential panel with multiple tests at one time. The same concept applies to other disease states, such as myositis, celiac disease, vasculitis, or antiphospholipid syndrome. We can generate several results—for example, 11 for the CTD Essential panel—from one cartridge instead of one at a time,” Manchester says.
New biomarkers that are included in the Aptiva menu will help close “the seronegative gap,” he says, but Werfen will do it in an automated fashion by combining it with its other existing markers. “So we’re moving forward with multiple tests in one cartridge but also using our chemiluminescence technology”—the Bio-Flash platform—“to push it forward.”
Werfen received FDA clearance in 2021 for the Aptiva Celiac Disease IgA and IgG assays and the CE mark for the Aptiva CTD Essential panel. “We’re marching forward with Aptiva assays for APS [antiphospholipid syndrome], rheumatoid arthritis, irritable bowel syndrome, myositis, vasculitis as well as autoimmune liver disease. We are expecting regulatory approvals throughout this year and beyond,” Manchester says.
With its Quanta Link data management system, he adds, they’re able to tie together the different technologies—indirect immunofluorescence (including Nova View), ELISA, chemiluminescence, and now Aptiva, the particle-based multianalyte technology (PMAT). “Consequently, we are able to deliver different technologies including immunofluorescence, the gold standard, in addition to chemiluminescence and PMAT. We are convinced that particle-based assays such as Bio-Flash and Aptiva represent the future in autoimmune testing.”

Falcetano
In allergy testing, allergen components are where the interest is, says Gary Falcetano, PA-C, Thermo Fisher’s clinical affairs manager for allergy-immunodiagnostics. The FDA in 2020 cleared the ImmunoCap specific IgE allergen component test for alpha-gal, and in 2019 it cleared the allergen component tests for stinging insects and pet allergen components. “Our allergists continue to ask for additional components and additional help in understanding the available components and how they can best use them to serve patients,” Falcetano says.
“Where the whole allergen extracts are great for sensitivity,” he says, “the components allow us to be more precise in the diagnosis.” Clinical history is always key to diagnosis, he adds, “but the allergen components take it to the next level.”
Thermo Fisher will continue to bring components before the FDA, he says, but, like so much else in laboratories, expanding menus has been secondary to SARS-CoV-2. “Everything tends to take a back seat to COVID testing, as it should,” he says, noting the staff shortage that predated the pandemic and is now acute.
Joshua Bornhorst, PhD, DABCC, Mayo Clinic consultant and assistant professor and co-director of clinical immunoassay laboratories, which includes allergy testing, presented a session at the AACC annual meeting last year on food allergy testing, where he called specific versus component IgE antibody testing “one of the current frontiers” of antibody IgE testing.
“When we talk about specific, we’re talking about the mix of all allergenic and nonallergenic proteins in an extract,” he said in the session. “So in some ways the title ‘specific’ antibody testing is a misnomer. It’s not just for antibodies against one protein, but rather a group of proteins extracted from that allergen. You don’t know which protein is involved because there are multiple proteins in that mixture. It’s called specific, though, because it is a specific extract of something.”
The next level is component allergen IgE antibody testing. “Now you can take individual components from that specific mixture, once you’ve identified them as the proteins or the chemicals that cause an allergic reaction,” he said. In the case of proteins, one can make a homogeneous mixture of purified or recombinant component, bind it to the matrix, and assess the ability to look for the antibodies against that specific component.
“These two can work hand in hand,” Dr. Bornhorst said.
The most common traditional multiallergen antibody panels are multispecific allergen panels. “You can take groupings of certain foods or epithelial allergens and run either combined assays or multiple specific assays for all of them. You can create a targeted panel”—food, food/nut, epithelia panels, for example—“to evaluate a set of clinical symptoms,” he said. It’s a more rapid approach to screening, it can rule out sensitization to multiple related allergens, and it offers flexibility in designing the panels in accordance with the preferences of clinicians. However, a positive result in combined assays does not identify specific allergen sensitization; thus it doesn’t always correlate with individual allergen testing. Even with multiple individual specific panels, he said, there is a lack of standardization among clinicians in the testing performed.
Common examples of existing or soon to be released component antibody panels are peanut, expanded nut, venom, egg, and animal dander and allergenic pet.
Egg component antibody panels are isolated components found in eggs, he said. There is a whole egg specific test that is a whole egg extract, and an egg white allergen-specific test, which is egg white extract. There is egg yolk, too. “And within those specific tests there are different components,” Dr. Bornhorst said. “We do have assays for two of those components: ovomucoid and ovalbumin.” Starting with whole egg, one can identify that the patient has an allergen to egg white and then dissect that further through the component test. “The difference between ovomucoid and ovalbumin is that ovalbumin is unstable,” he said, “so things that are highly processed or cooked—if you have an ovalbumin allergy—should be relatively safe. If you have an ovomucoid, cooking the egg won’t affect your allergic response.”
Individuals who identify as having an egg yolk allergy are often found to have a kind of asthma due to inhalation of bird dander. “It’s not perfect,” he said, but “if you use the available tests—both specific and otherwise—you can generate a clinical picture.”
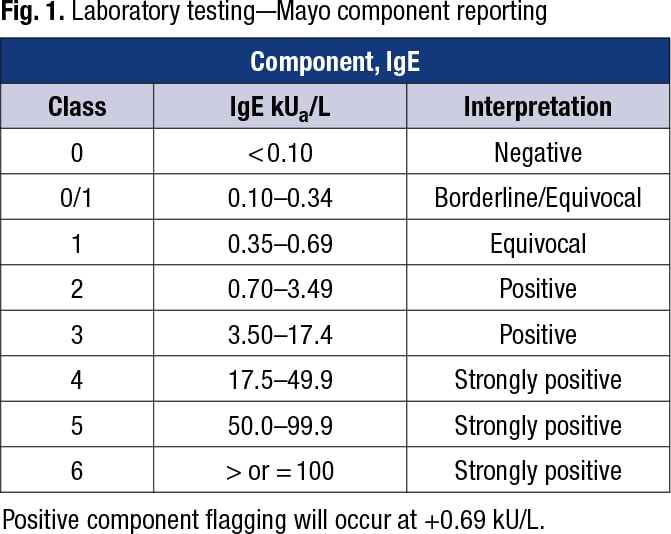
For component test reporting at Mayo Clinic, “we report down to 0.10 kU/L,” Dr. Bornhorst said (Fig. 1).
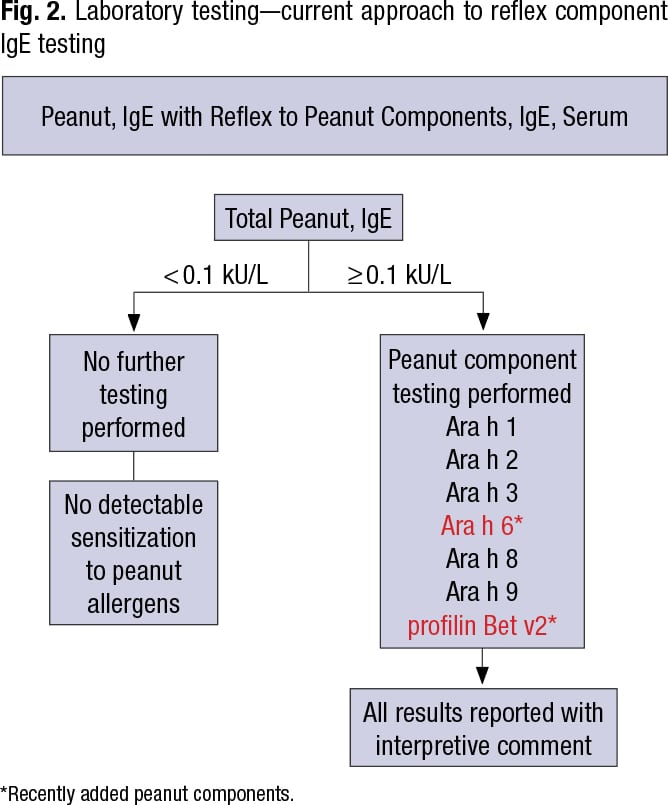
For peanut component antibodies, Mayo Clinic traditionally has tested for five main components—Ara h 1, 2, 3, 8, and 9—which are the most allergenic of the 30 peanut proteins, 18 of which are associated with sensitization, he said. However, the major component proteins account for about 90 to 95 percent of peanut allergy.
Mayo Clinic recently added two peanut components—Ara h 6 and profilin Bet v2—to its menu. “Profilin Bet v2 is a more cross-reactive protein,” Dr. Bornhorst said in an interview, “and the other, Ara h 6, is similar to a preexisting protein component [Ara h 2] within the previous five-component panel. The addition of more complements is intended to improve the sensitivity of peanut component testing relative to the overall specific total peanut IgE extract assay.”
“So you have a mixture of proteins, you do your specific total peanut test. If it’s positive you reflex to component testing, and then you report that with an interpretive comment.” It’s a mixture of specific at the start and component testing to generate a clinical picture (Fig. 2).
One reason for this, he said, is that different components have different resistance to digestion and heat and different amounts of severity, which can guide patient allergen avoidance or treatment. Ara h 2 is often considered to be the most severe allergen in terms of allergic response severity.
Oral allergy syndrome is a type of food allergy in which allergic reaction occurs in the mouth after eating certain fruits, nuts, or vegetables, including peanuts, he said. It’s associated with cross-reactivity of Ara h 8 (a Bet v1 homologue that is cross-reactive with birch pollen allergen) and Ara h 9 (a nonspecific lipid transfer protein that is cross-reactive with pitted fruit allergen). Thus, component testing can be used to differentiate different types of potential allergenic response.
A comparative study of diagnostic test characteristics of the peanut skin prick test, peanut-specific IgE serum antibody testing, and IgE antibody testing for peanut components, in a screening population of 321 infants before known peanut exposure, revealed that Ara h 2 is the most specific allergen, Dr. Bornhorst said (Keet C, et al. J Allergy Clin Immunol. 2021;147[3]:977–983.e2). At a cutoff point of 0.1 kUa/L, Ara h 2-sIgE discriminated between allergic and nonallergic best. Total peanut IgE was found to be the most sensitive but not nearly as specific. “So there are advantages of considering using Ara h 2 as a frontline test, in some populations, or as is done in Mayo peanut component reflex panel testing—testing for total specific IgE first, and then reflexing to subsequent component testing to increase overall sensitivity for allergic reaction,” he said.
Because the specificity of “specific” assays is not 100 percent, Dr. Bornhorst advises against the routine use of large screening panels or annual testing on an individual without clinical indication of allergy. “You will get false-positives.”

Dr. Bornhorst
In addition to its launch of Ara h 6 and profilin Bet v2, Mayo Clinic recently launched its bromelain MUXF3 testing to evaluate for the presence of antibodies to cross-reactive carbohydrate determinants. CCD structures are found in plant and insect glycoproteins and are commonly recognized by IgE antibodies as epitopes that can lead to widespread cross-reactivity to different allergens and potentially cause false-positives in in vitro diagnostic serum IgE antibody testing results (Sinson E, et al. PLoS One. 2020;15[4]:e0231344). “There’s increasing interest in some platforms as to what degree of cross-reactivity or interference you may see in positive serum IgE antibody results due to these cross-reactive determinants. So there’s interest in designing assays away from that and then also including such things as cross-reactive inhibitors and blocking agents,” Dr. Bornhorst tells CAP TODAY.
IgE antibodies against bromelain is a test for this cross-reactivity since its MUXF3 carbohydrate chain is found in many plant proteins, including peanuts. Sinson, et al., analyzed sera from patients sensitized to peanut, silver birch, and/or timothy grass against the MUXF3 serum IgE, and as much as 35 percent of the sensitized group tested in the study was found to be reactive to CCD allergen (≥0.35 kU/L), Dr. Bornhorst said.
“There is some growing evidence that CCDs cross-react and cause multiple false-positives in serum IgE antibody testing, and it may be dependent in an instrument platform- and assay/allergen-specific manner,” he said. The interest in CCD inhibitors, blocking agents, and assay markers of CCD interference is growing, he said, but CCDs generally don’t cause clinical allergic reaction.
Miguel Park, MD, allergist-immunologist, internist, and assistant professor at Mayo Clinic, said in the AACC session, in which he was a co-presenter, that the history of the reaction is one of the drivers of whether to test, and risk factors and allergen prevalence, too, factor into the pretest probability. Then it’s a question of posttest probability: “Will the skin test or IgE serum testing, whether it’s component or whole or even the oral challenge, further our pretest probability to a higher probability?”
Dr. Park reported on the case of a 13-month-old male patient who was seen for a possible peanut allergy. Clinically (and with repeated exposures), the pretest probability that the patient had a peanut allergy was high. Dr. Park ordered a blood test for the patient, and the result was an IgE of 7.65 kU/L (in the positive range). How to interpret these tests is the question, he said. If the pretest probability is high and the skin test or serum IgE test is positive, then it helps confirm the diagnosis. However, if the pretest probability is low and the skin test or serum IgE test is positive, then the testing may not help in the diagnosis. Positive skin prick and serum IgE tests may indicate sensitization but do not alone equate to clinical diagnosis. “As clinicians, we think of these tests as having high sensitivity but low specificity.”
Cutoffs have been developed for certain foods, and while they’re “wonderful to have,” Dr. Park said, caution is needed because they were established in tertiary medical center studies in patients with moderate to severe atopic conditions (e.g. severe atopic dermatitis) and with extensive family history. “It makes you wonder about their generalizability and whether they’re relevant to your patient population.”
Some studies have suggested that component testing has high specificity and positive predictive value and could make it unnecessary to do an oral challenge, Dr. Park said. It may have an advantage in situations in which the patient is sensitized without a history of clinical reaction, or when skin and serum tests are discrepant. “And possibly it might help predict the severity of the reactions in the future,” he said. It also has much better specificity than skin testing or specific IgE testing to particular foods (Anagnostou A. Ann Allergy Asthma Immunol. 2019;122[6]:576–579).
The limitations of component testing can be seen in the variabilities in cutoffs (Flores Kim J, et al. Allergy. 2018;73[8]:1609–1621), sensitivity, specificity, and positive and negative predictive values. “It kind of makes you argue that maybe we’re not ready for prime time with these tests,” Dr. Park said.
Professional societies have been trying to find a way to merge the clinical history with component testing, he said, and one group advocated for using likelihood ratios to go from pretest to posttest probability (Greenhawt M, et al. J Allergy Clin Immunol. 2020;146[6]:1302–1334). “It’s not dependent on population prevalence of disease, and they think it’s more adaptable to individual clinical settings,” he said.
Greenhawt, et al., wrote that diagnostic testing (skin prick or serum IgE) should not be used in patients in whom there is low or very low pretest probability of peanut allergy. “The bottom line,” Dr. Park said, “is that if a patient has a high pretest probability, they’re giving us clinicians the go-ahead to use any of them—skin, blood, Ara h 2 component tests” within the Fagan nomogram. But they caution against the routine use of component testing in addition to either skin testing or serum-specific IgE to whole peanut to increase diagnostic accuracy.
Amy Carpenter Aquino is CAP TODAY senior editor.