Karen Titus
February 2020—Human endeavors are bursting with unintended consequences. Kudzu comes to mind. Smokestacks. Some even point fingers at Smokey Bear.
John Greden, MD, offers an example of his own, one with renewed relevance in pharmacogenomics. It’s a subject he’s studied closely, including as principal investigator of the GUIDED trial (Greden JF, et al. J Psychiatr Res. 2019;111:59–67). Researchers looked at whether offering clinicians access to a pharmacogenomics test report would improve treatment for more than 1,100 patients with a major depressive disorder who had already failed to respond to an average of 3.5 antidepressant trials.

Philip Empey, PharmD, PhD, with Annerose Berndt, DVM, PhD, director of the UPMC Genome Center. “If the data’s available,” Dr. Empey says of pharmacogenomics, “I’m definitely on the we-should-be-using-it side of things.” (Photo: Scott Goldsmith)
Physicians with lengthy memories should find nothing revolutionary about using laboratory testing in mental health, says Dr. Greden, the Rachel Upjohn professor of psychiatry and clinical neurosciences, Department of Psychiatry, and founder and executive director, University of Michigan Depression Center. In the era of tricyclic antidepressants, physicians monitored plasma levels in patients fairly routinely. Says Dr. Greden, who chaired Michigan’s Department of Psychiatry from 1985 to 2007, “There was evidence early on that if you didn’t have an adequate plasma level, people did not improve.” Too high a level, moreover, was dangerous for patients who were poor metabolizers.
The pages began to turn with the publication of Prozac Nation in 1994, which helped popularize fluoxetine and other selective serotonin reuptake inhibitors, Dr. Greden recalls. SSRIs are effective and don’t have the same risks—cardiac problems, orthostatic hypertension, etc.—that accompanied overly high levels of tricyclics.
But with that came an uncoupling of lab testing and depression treatment that, in retrospect, seems a bit unfortunate, Dr. Greden says. “There were some real clinical advantages in measuring plasma levels,” he says. In achieving safety and comparable efficacy—goals no one would argue with, of course—medicine may have derailed early momentum toward precision medicine.
“Now it’s going to take some work to get the mental health delivery system, at least, to start thinking along the lines of, What lab tests should I consider before I even make my drug choice?” says Dr. Greden, who is also founding chair, National Network of Depression Centers, and research professor at Michigan’s Molecular and Behavioral Neuroscience Institute.
But it’s work worth doing, he and others say, whether that means stepping forward or finding a way back.
Not every clinical condition lugs the same historical baggage when it comes to pharmacogenomics. Philip Empey, PharmD, PhD, associate professor, University of Pittsburgh School of Pharmacy, Department of Pharmacy and Therapeutics, says, “I see more and more academic institutions starting to initiate larger, broader projects to guide us in therapy. Notwithstanding reimbursement issues—those are real—to overcome those issues, the best thing we can do is generate real-world data of clinical utility.”
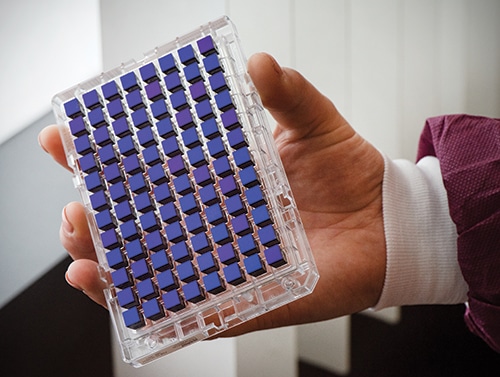
Each assay on the Thermo Fisher PharmacoScan array can test more than 4,600 markers in nearly 1,200 genes for a single sample, including copy number for targeted genes. The plate allows for testing of up to 96 patients simultaneously. (Photo: Scott Goldsmith)
His institution continues to charge ahead, building on earlier work. In 2015, Pitt/UPMC began a clinical implementation program focused on the role of CYP2C19 in clopidogrel (patients who are classified as CYP2C19 intermediate or poor metabolizers are unlikely to benefit from the antiplatelet drug), with about 3,000 patients assessed so far. Dr. Empey, who is also associate director of the Pitt/UPMC Institute for Precision Medicine, makes a rosy report: “That’s worked well, with strong payer reimbursement and great feedback from clinicians and patients.” Dr. Empey spoke about their work and PGx testing at the Association for Molecular Pathology annual meeting in November.
More recently, Dr. Empey and colleagues are deploying, through Pitt’s newly established Pharmacogenomics Center of Excellence (of which he is director) and the Clinical and Translational Science Institute, preemptive population-based screening as a part of a Pitt/UPMC research study.
This is a large biobanking project, called Pitt+Me Discovery. Enrollees have the option to receive their pharmacogenomic results (an increasingly common offering at medical centers throughout the country; see “Genetics lands in primary care inboxes,” CAP TODAY, June 2019). For those who opt in, clinically actionable pharmacogenomic variants from the panel will be entered into the medical record and, not incidentally, made available to prescribing caregivers across the UPMC system.
About 5,000 patients—of a targeted 150,000—have been enrolled so far, Dr. Empey reports. The majority of the validation work in the clinical laboratory, the UPMC Genome Center, has been completed, “but we have not yet returned results to the medical record. There’s lots to build in that process, including clinical decision support.”
Though open to any interested UPMC patient, “We believe there’s stronger value in the return of pharmacogenomic results when there’s prescribing or conditions that are likely to have clinical utility,” Dr. Empey says. In other words, they prefer to get their hits with runners already in scoring position. “We’ve started doing analysis within our electronic medical records to understand where prescribing of these medications is highest and where the strongest benefit is. We’ll target recruitment in those areas.”
That’s the dream. Reality often steers ships in other directions, however, and Dr. Empey is well aware that the views of both his colleagues and patients will shape how pharmacogenomics develops.
“When we talk to patients,” Dr. Empey says, “they often assume all drugs can be guided by these new technologies.” Obviously that’s not the case.
If patients are the sunny Maria von Trapp in this scenario, physicians are the dreary Baroness. “When we talk to clinicians in general, they have the opposite opinion,” says Dr. Empey. Their view? Pharmacogenomics is not ready, with little data to support its clinical use.
In reality, as Dr. Empey noted during his AMP talk, nearly 300 medications have some mention of pharmacogenomics in their FDA product labeling. “I don’t want to oversell that,” he says, noting that in some cases that mention might fall quite low in the labeling. “But I use that statistic to get people excited that there actually is quite a bit of data in regulatory guidance. In reality, there’s 30 to 40 medications where there’s strong guidance on how to use testing results if they are available.”
PharmVar (www.pharmvar.org) is a useful resource for laboratories trying to understand varying allele definitions. PharmGKB (www.pharmgkb.org) is another well-established site for annotations and aggregating regulatory information, among other things.
But the real mother lode is the Clinical Pharmacogenetics Implementation Consortium (https://cpicpgx.org), a resource he mentions repeatedly, like a slogan at a rally. “Everyone should be aware that there are peer-reviewed consensus guidelines on the appropriate use of pharmacogenetic data to guide prescribing and of all the great work that CPIC does,” Dr. Empey says. “The more people are aware of these freely available guidelines, the better we all are as a field about knowing how to use the information appropriately in clinical care.”
Dr. Empey uses the chicken-or-egg reality to describe the current conundrum in the field. One approach is to build evidence-based arguments to justify PGx testing using current costs and projections of value of these data. But in reality, he says, “The guidelines are ahead of that, and imagine a time when these data are ubiquitous—saying that when the data is available, this is how you should use it.”
Institutions will need to decide for themselves when it makes sense to start building the infrastructure to support PGx testing. UPMC, obviously, has reached that tipping point—hence its large population-based study.
He calls himself an optimist—clearly, those hills are alive—and says he likes where the field is heading. Without ignoring the need for more real-world data, he says, “If the data’s available, I’m definitely on the we-should-be-using-it side of things.”
That physician-patient fissure is an interesting place to pause.
Patients’ experiences with their medications can resemble encounters with the law—supportive for many, bruising for others. Patients who are frustrated by side effects, costs, etc., may look for other solutions. Pharmacogenomics will not provide answers in every case, Dr. Empey acknowledges, but for someone who’s paying hundreds of dollars or more a month for an antidepressant, say, or antiplatelet medication that might not be working, the allure is appreciable. “You can imagine someone saying, Well, this is a pretty logical solution. Why wouldn’t we do this?”

For Pitt+Me Discovery, the majority of the validation work in the clinical lab, the UPMC Genome Center, has been completed, “but we have not yet returned results to the medical record,” Dr. Empey says, adding, “There’s lots to build in that process, including clinical decision support.” Above, a multidisciplinary team of the UPMC Genome Center and the University of Pittsburgh School of Pharmacy. Clockwise from left: Dr. Empey; Keito Hoshitsuki, PharmD; Lindsey Kelly, PhD; Karryn Crisamore, PharmD; Dara Kozak; and Annerose Berndt, DVM, PhD. (Photo: Scott Goldsmith)
Some clinicians and payers launch from a different angle. Their starting point, Dr. Empey suggests, is, When is it something that I need to do in everybody?
In between lies an opportunity. Dr. Empey’s own institution has joined the slowly growing ranks of sites that offer pharmacogenomics clinics, where patients who are seeking PGx-guided care can talk with a pharmacist and physician familiar with the data—and who will order testing if warranted.
Patient interest is also growing thanks to DNA ancestry testing, a business that has been eyeing health-related testing of late. Health care in general has become much more consumer directed, Dr. Empey observes. “But sometimes our field is critical of direct-to-consumer companies for being outside the clinical environments. In many ways, though, they’re helping to stimulate an important consumer mindset—activating patients to be more and more active in their own health—and that’s a good thing.” For patients, it makes sense to take available genetic information and seek a caregiver and laboratory that will help them understand it, rather than await “a more paternalistic push down from a clinician.”
Dr. Empey sees a chance to seize on that momentum and create an educated audience. His Test2Learn program wrestles with what he calls “the biggest bear” in moving pharmacogenomics forward: How to train the clinicians already in practice?
Interested learners can optionally undergo the genotyping process themselves, and then consider using their own data in their coursework. The program has been deployed in the Pitt School of Pharmacy curriculum for six years and is now offered in nationally deployed certificate and continuing education programs for practicing pharmacists and physicians as well. Dr. Empey’s team has reported strong learning outcomes from this approach.
It’s also possible that patients’ encounters with personalized, PGx-driven medicine will result in more patient satisfaction—a success metric in and of itself. It could also be cost-effective in a more traditional sense. And it could improve patient adherence if it connects patients to a drug that works better, has fewer side effects, or both.
In the midst of all this, Dr. Empey sees an opening for laboratories. “There’s a great role for labs,” he says. In addition to providing high-quality testing and interpretation, “labs can be front and center in emphasizing that these services exist.”
Putting pharmacogenomics testing to work remains an uphill journey—prepare to climb a lot of mountains, if not every one. Dr. Empey and others reported on 12 early adopters of CYP2C19 genotype-guided antiplatelet therapy (Empey PE, et al. Clin Pharmacol Ther. 2018[4];104:664–674). Their experiences provide useful insight into what can make a PGx endeavor sink or swim, he says.
Foremost, “You need a clinician champion to be able to start programs. If you have a great lab or a great research group and you don’t have that [clinical] champion to spearhead implementation, they’re a lot harder to get off the ground.”
Education, as noted, is also critical. Those involved need to know about CPIC and other available resources. As knowledge expands, so will the field. Just as there’s no need to explain to anyone that a poor renal function may require changes in dosing of some medications, he foresees a day when knowing that someone is a CYP2C19 intermediate metabolizer will automatically drive downstream action.
At the same time, “You don’t want to underappreciate the work involved in the informatics piece,” Dr. Empey warns. “That really is what often takes the bulk of the time in setting up these programs.” Pharmacogenomics requires integrated information. Labs need to figure out how to transfer data in a discrete way that will feed into decision support systems—sending a coded set of fields using standard terms, for example: This person was tested for CYP2C19, their genotype was CYP2C19 *1/*2, and they are a CYP2C19 intermediate metabolizer. “We take those three database fields of information and place them in the medical record and use those fields to trigger decision support.” Flagging an entire report as normal or abnormal is virtually useless when large panels are involved because the frequencies of variants are too high.
How much interpretation might be required? Opinions vary, and it’s an area of debate in the PGx field with the FDA and laboratories. The agency seems to be suggesting that reports should be less drug based and more genetics based, Dr. Empey says, while leaders in the field suggest that this information alone might be difficult for everyone to use.
The UPMC laboratory is on site, and it reports only genotype and phenotype; there are no drug-based recommendations. “And that’s fine,” Dr. Empey says, “because those are carried out within our electronic medical records and downstream pharmacist-led clinical services.”
But that model would not work as well with an external laboratory that provides reports directly to physicians, he says, since they may not know automatically what to do with the data.
For Dr. Empey, the game is already afoot, but he knows not everyone is ready to embrace pharmacogenomics. Some people might feel burned by their previous enthusiasm. “There were people who were very passionate about it in the ‘90s, who are perhaps more jaded right now—you know, they tried this for years and it hasn’t happened.”
As with the evolution of fake meat, perhaps this time the hype is real (so to speak). No amount of wishful thinking (or numbed taste buds) were enough to convince diners that a Boca Burger and a beef patty sizzling on the grill were peers. Today, however, maybe the Impossible Burger is up to the task. “I’m really enthusiastic that we’re going to cross the threshold this time for broad-based deployment,” Dr. Empey says.
At the same time, he urges a cautious approach—no need to gobble up everything in sight. “Because sometimes we have folks who are overenthusiastic in interpreting the data, too—that if you see someone who’s a rapid metabolizer, that must mean you increase their dose.” Dr. Empey worries other aspects will be lost in such zeal. “Genetics is just one piece of the puzzle. You can override phenotypes predicted by genetics with drug interactions and other clinical factors. So we find ourselves continually championing the field but also tempering it.”
At this point, where should labs start? Should they catch another boat mid-cruise, or start flinging off lines at the dock and head out to sea on their own?
It depends, says Dr. Empey. “Know your audience,” he advises. At his institution, initial aspirations were big: a large panel for their very first test. After further reflection, they scaled back to the simple, single CYP2C19 gene. The benefits were still there, “and we learned a tremendous amount about how to effectively implement.” Though he understands the temptation to think big, he advises labs to peruse CPIC and PharmGKB data. “Testing a bunch of genes with low-quality evidence on the report doesn’t make it better.”
Educated restraint will help the field as well as individual institutions, he adds. He worries about scope creep: If testing 16 genes is good, 30 must be better. And imagine 120! “You end up with a lot of data that isn’t useful—at least not right now—and it ends up making it more difficult for clinicians and payers to see the value in the product.”
“Sometimes enthusiasm outpaces our ability to generate the data,” Dr. Empey says. He points to early excitement over pharmacogenomics-based testing for warfarin, a medication known to have genetics associations with both its metabolism and its target, VKORC1. In the late 2000s a number of institutions launched PGx testing programs, but subsequent studies offered a mixed view of its value. Some European studies were positive, but a U.S.-based trial was more equivocal, he says. “That put some cold water on reimbursement.” Several years ago, however, another large, positive, randomized controlled trial reported genotype-guided warfarin dosing, compared with clinically guided dosing, produced better outcomes after hip and knee surgeries. “So the pendulum goes back and forth.”
Michigan’s Dr. Greden knows which way he’d like the pendulum to swing. “Will this start to come into play?” he asks. “I certainly hope so. Because these tests are needed.”
Their potential for use in treating brain behavior illnesses (his preferred term) may not be fully appreciated, he says. Clinical depressions alone are ranked by the WHO as the No. 1 disabling illness worldwide, he says, with a lifetime prevalence of about 17 percent. Untreated or not adequately treated to remission, clinical depressions tend to be episodic and recurrent, worsening over time. Of patients with a well-diagnosed major depressive disorder, only about 37 to 38 percent achieve remission with the doctor’s first treatment. And treatments are incredibly costly.
The picture should not be so grim, he posits, with more than 40 antidepressants available, not to mention other interventions. “So why do we have such horrible figures?”
A large (4,041 outpatients) National Institute of Mental Health-funded study from the early 2000s, the STAR*D trial (Sequenced Treatment Alternatives to Relieve Depression), looked at treatment of patients with depression who didn’t respond to their initial medication. Of those who then tried another or added treatment, 30 percent more responded. Those still struggling were offered two additional levels of treatment, if needed. One year after treatment initiation, 30 percent were still struggling. Says Dr. Greden: “We call those treatment resistant.”
That’s Dr. Greden’s area of interest and expertise. Clearly more precise treatments were needed. “But historically we didn’t have many clues to enable us to do that better,” he says.
In treating his own patients, he observed that many couldn’t tolerate a medication’s severe side effects. “I’d say, ‘Uh-oh, we have a poor metabolizer.’” Other patients who felt no effects asked if they’d been given a placebo, indicating they were rapid metabolizers. In other cases, patients would respond well for several weeks, and then side effects would start to appear. “I’d think, We’ve got an intermediate but relatively slow metabolizer, and now it’s caught up.”
That was the state of things decades ago, when the tricyclics were being measured. “That helped, but you were targeting one medicine. And there was still nothing that told you what not to do,” he recalls. Meanwhile, he was watching oncology and other fields start to take a hard look at pharmacogenomics.

Dr. Greden is eager for the day when PGx testing in brain behavior illnesses begins to keep up with the advances made in oncology and other fields. “But in the meantime,” he says, “if you ask, Is it clinically valuable now? I would say yes.”
In his field, it became clear that no single gene or metabolic pathway was going to provide any answers. In about 2011, Dr. Greden, on behalf of the National Network of Depression Centers, was approached by Assurex Health (since purchased by Myriad Neuroscience) to do a large-scale study. Dr. Greden became the PI of the GUIDED study—involving eight genes and 28 medications—to guide treatment using a combinatorial model in patients who’d failed earlier treatments.
“So right away we were dealing with a difficult population,” Dr. Greden says. More than 2,000 people were screened at multiple sites, with more than 100 doctors involved. Patients were randomized into either the treatment-as-usual group, where prescribing physicians chose their favored treatment, or the guided care arm, where physicians had access to the PGx testing results and could use them to help make their treatment decision (though they weren’t required to).
The guided arm achieved better results, says Dr. Greden. “What these tests did was probably help the doctor by saying, ‘There are some medicines you do not want to use.’” Close to one in five patients had incongruent medications, Dr. Greden reports—that is, one in five people getting treatment as usual were given a medication that was a poor choice for them, given their gene composition and metabolic pattern.
Did that make a difference? The short answer is yes. Those who received congruent medications did significantly better in terms of symptom response and remission. While the test results didn’t tell physicians which drug worked best, it helped “warn you about which ones you should stay away from,” Dr. Greden says.
An equally important clinical question was, If pharmacogenomic testing information is conveyed to clinicians, do they actually change? “Basically, the answer is, doctors can, and do, change,” says Dr. Greden—to a pretty dramatic tune. Some 79 percent of patients in the guided care arm were on incongruent medications at the start of the study; at study’s end, only 10 percent were. That group responded better, as noted; moreover, their side effects decreased—6.5 percent of those who switched from an incongruent to a congruent medication reported side effects, compared with 16.5 percent of those who remained on an incongruent medication.
The study was continued for 24 weeks (though the blind rating was broken). Patients on guided therapy continued to steadily improve. “One curve goes up; the other doesn’t,” he says, noting that the latter stage was an open design, with the blind broken at eight weeks. Again, he finds this encouraging, given that these are long-term, even lifetime, illnesses. Furthermore, equally good test results were found among the aged population with major depressions. Also interesting, he says, is those who were on incongruent medications had a higher rate of discontinuation.
If PGx testing is helpful for treatment-resistant patients, could it also be used earlier? His own view has shifted from the testing being a tool for those with treatment resistance to using pharmacogenomics testing before initiating treatment. “It would likely be useful, decreasing disability, perhaps saving lives and costs. I say that simply because these are such disabling illnesses.” But “we don’t have the answer, because that study hasn’t been done yet,” Dr. Greden says. But such a study could answer the question every physician seems to ask of every lab test: What do I do?
That’s not the only study Dr. Greden would like to see. More studies—more studies! Larger studies. Longer studies. Children and adolescents. Ethnic differences. Substance misuse. Gender differences. Whether the number of episodes affects response. “And I especially want to know: Can pharmacogenomics tests actually be beneficial in helping doctors identify who’s at greatest risk of suicide? We have not addressed that adequately,” says Dr. Greden. And depression is only one focus. Bipolar and anxiety disorders, among others, are also in need of better treatment guidance, he says.
Dr. Greden is eager for the day when PGx testing in brain behavior illnesses begins to keep up with the advances being made in oncology and other fields. “But in the meantime, if you ask, Is it clinically valuable now? I would say yes.”
Like Dr. Empey, Dr. Greden encounters his share of skeptics. And like Dr. Empey, Dr. Greden plants a flag on the hill of education.
Says Dr. Greden: “The skeptics are the ones who start out with an accurate criticism, but a misunderstanding of lab test development. They say, ‘I want to know what I’m supposed to do. Don’t tell me what I’m not supposed to do.’”
“That’s got to be overcome with education,” he continues. “I’m sure lab folks have to live with this all the time.”
Dr. Greden points out that the majority of people with clinical depression are treated by nonpsychiatrists—internists, family medicine specialists, pediatricians, obstetricians, college mental health providers. Interestingly, he’s found that primary care providers often end up being more receptive to the idea of using pharmacogenomics to help them make decisions.
He’d also like to see hospital-based laboratories carve out a role in this area. “It’s really important for pathologists and laboratory directors to buy into the wisdom of the need for this testing, and take the lead to do this in a standardized way.”
He’s been engaging with the subject regularly, including at seven grand rounds and as a keynote speaker at the upcoming American Psychiatric Association meeting. The common questions he hears include: Are these tests approved? Is the FDA behind this? Is this just a research tool? What is the actual cost? Does it save money or cost money? Does insurance pay for this? Is there confidentiality? How do I choose the right test?
One area where he’s had less discussion, curiously, has been closer to home. “We have begun talking about this at the University of Michigan in family medicine, internal medicine, OB-GYN, et cetera, but have much more to do,” he says. In fact, he’s hoping to renew discussions he first tried to have a few years ago. “I tried to bring it up, but everyone said the tests weren’t very good, and there was some truth to that.”
Talking with CAP TODAY might be the right impetus, he says. “I can say, ‘Clinical pathologists are looking at these things. Maybe it’s time major medical centers do more of it in their own backyards.’”
Karen Titus is CAP TODAY contributing editor and co-managing editor.