Editor: Frederick L. Kiechle, MD, PhD
Submit your pathology-related question for reply by appropriate medical consultants. CAP TODAY will make every effort to answer all relevant questions. However, those questions that are not of general interest may not receive a reply. For your question to be considered, you must include your name and address; this information will be omitted if your question is published in CAP TODAY.
“Q&A” is devoted this month to a question about HER2 testing in colorectal cancer.
Q. I am a community pathologist and would like to know if the CAP has recommendations on diagnostic criteria for evaluating HER2 in colorectal carcinoma. There appears to be more than one set of criteria in various references (i.e. HERACLES, Ventana), and when clinicians request the test, I am not sure how best to evaluate these specimens.
A. February 2020—The CAP has no official position on HER2 testing in colorectal cancer. The following represents expert opinion based on my experience as an immunohistochemistry laboratory director and longtime member of the CAP Immunohistochemistry Committee and my careful review of the literature. This response was peer reviewed by other GI pathologists on the Immunohistochemistry Committee. I will discuss the HERACLES and so-called Ventana diagnostic criteria and other aspects germane to HER2 testing in non-breast/non-gastroesophageal carcinomas. Of note, anti-HER2 therapy is only FDA approved in breast and gastric/gastroesophageal junction adenocarcinomas, and treatment of other HER2-positive carcinomas should be considered only in patients who have failed conventional therapies and/or in the context of a clinical trial.
Two recent phase two clinical trials demonstrated moderate activity of dual anti-HER2 therapy in advanced colorectal cancer. The HERACLES (HER2 Amplification for Colorectal Cancer Enhanced Stratification) trial enrolled 27 KRAS wild-type, HER2-positive patients for treatment with combined trastuzumab (a monoclonal antibody to extracellular subdomain IV of HER2) and lapatinib (a small-molecule inhibitor of HER2 and EGFR). Eight (30 percent) patients achieved an objective response, including one complete response and seven partial responses; 12 additional patients had stable disease.1 HER2 positivity was defined by the HERACLES Diagnostic Criteria, formulated specifically to select patients for this clinical trial; testing was performed centrally.2
MyPathway is a phase two multiple basket trial, enrolling patients with diverse solid tumor types for targeted anti-HER2, BRAF, EGFR, or Hedgehog signaling pathway therapy. Investigators reported on 57 HER2-positive advanced colorectal cancer patients, enrolled regardless of KRAS status, treated with combined trastuzumab and pertuzumab (a monoclonal antibody to extracellular subdomain II of HER2, which inhibits HER2/HER3 dimerization). Eighteen (32 percent) patients achieved an objective response, including one complete response and 17 partial responses; seven additional patients had stable disease for greater than four months.3 HER2 positivity was defined as any of the following: 1) HER2 IHC 3+ in >10 percent of cells, 2) HER2:CEP17 ratio ≥2.0 or HER2 count >6 per cell, 3) increased HER2 gene copy number by molecular methods, and/or 4) HER2 activating mutations, including exon 20 insertions; deletions around amino acids 755–759; G309A, G309E, S310F, D769H, D769Y, V777L, P780-Y781insGSP, V842I, R896C; or previously reported activating mutations (or indels) in COSMIC. HER2 testing was performed by local CLIA-certified laboratories.
Pathologists have expressed confusion about which HER2 testing criteria to apply in colon cancer. I have also heard pathologists say they have been told not to use gastric/gastroesophageal junction criteria. The HERACLES criteria were designed to select patients for a clinical trial. Implicit here is the goal to have a positive clinical trial. A (unprecedented) 50 percent threshold for IHC positivity was established in a cohort of only 17 positive cases.2 The 50 percent threshold optimized the accuracy of positive Ventana Pathway (FDA-approved kit) immunohistochemistry to predict ISH positivity, which was also set at an unprecedented 50 percent cellularity threshold. These same cases were also examined using the Dako A0485 polyclonal antibody with immunohistochemistry performed manually. Using this assay in the same set of cases, a 10 percent positive threshold was most accurate. Nevertheless, the authors decided to implement a 50 percent threshold for the clinical trial.
For the purpose of identifying the most patients who would potentially benefit from a therapy, I found these criteria to be overly restrictive. I was also concerned that the results of testing generated by a central laboratory would not necessarily be generalizable. After the ToGA trial in gastric/gastroesophageal junction cancers, there was opportunity to further evaluate the interlaboratory and interobserver reproducibility of trial-derived HER2 testing criteria.4 All that said, before the publication of the positive MyPathway trial, these were the only criteria that were clinically validated.
The only reference I could find to Ventana colorectal cancer HER2 testing criteria is in an excellent review of the state of the bench-to-bedside science of HER2 in colon cancer,5 coauthored by many of the authors of the HERACLES clinical trial.1 In the table in which they list the Ventana criteria, they reference a review article on HER2 testing in gastric cancer6 by some of the same authors of the HER2 testing guidelines developed in the setting of the ToGA trial7—that is to say, the Ventana colorectal cancer HER2 criteria are equivalent to those used in resections of gastroesophageal adenocarcinomas (which may be variously referred to as ToGA or Ruschoff/Hofmann criteria and which were adopted in the CAP/ASCP/ASCO gastroesophageal adenocarcinoma HER2 guideline).8 The MyPathway trial used these latter, less restrictive criteria, along with a couple of novel molecular ones. I use these criteria in my practice.

Table 1 compares the CAP/ASCP/ASCO gastroesophageal and HERACLES colon HER2 immunohistochemistry criteria. In bold are the areas where the interpretation or subsequent testing/clinical consequences differ. In many cases, these are the same. Both sets of criteria recognize lateral membrane and basolateral (U shaped) staining as potentially positive staining patterns. The HERACLES criteria assign patients with weak to moderate specific staining in 10 to 49 percent of tumor cells to the negative category; according to CAP/ASCP/ASCO criteria, these tumors should be tested by in situ hybridization (ISH). The HERACLES criteria dictate repeat IHC in tumors with 2+ staining in ≥50 percent of tumor cells, while by CAP/ASCP/ASCO criteria, one would proceed directly to ISH. Similarly, the HERACLES criteria specify repeat IHC in tumors with 3+ staining in 10 to 50 percent of tumor cells, as well as confirmatory ISH, while by CAP/ASCP/ASCO criteria, these would be considered positive.
My main concern with the HERACLES IHC criteria is that they deny patients with IHC 2+ staining in 10 to 49 percent of cells the opportunity to be positive by ISH. In the initial HERACLES validation study, one of the 17 ISH-positive tumors showed 2+ staining in 20 percent of cells using the A0485 antibody.2 These criteria also dictate repeat IHC testing in scenarios in which one might otherwise proceed directly to ISH or consider a case positive, as well as additional ISH in one scenario (i.e. 3+, ≥10 percent) otherwise typically considered positive by IHC alone.
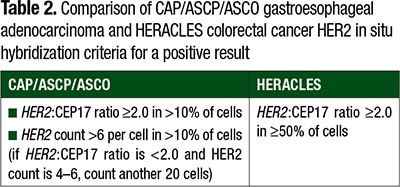
Table 2 compares the CAP/ASCP/ASCO gastroesophageal and HERACLES ISH criteria. The HERACLES criteria again set a positivity threshold as amplification in ≥50 percent of tumor, while the CAP/ASCP/ASCO threshold considers amplification in >10 percent and allows for positivity in instances in which the HER2 count is >6 per cell, even in the absence of a HER2:CEP17 ratio ≥2.0 (a scenario that may occur due to co-amplification of HER2 and CEP17). These latter, more permissive criteria were used in the MyPathway trial.
I was interested in the impact that increasing the threshold for IHC positivity from 10 to 50 percent might have on clinical testing. This depends, of course, on the frequency of this extent of staining in a given tumor type, which reflects a tumor’s tendency for heterogeneity of HER2 overexpression. In breast cancer, HER2 expression tends to be uniform. Thus, changing the threshold for positivity from 30 percent to 10 percent (per ASCO/CAP 2007 and 2013 guidelines, respectively) has had little effect on rates of IHC 3+ (ranging from increases of 0.5 to 1.5 percent in the three studies I could find that applied 2007 and 2013 IHC criteria to the same cohorts).9-11 Gastroesophageal adenocarcinomas are inherently more heterogeneous, with up to 30 percent of HER2-amplified cases having <30 percent cells staining by IHC.6 In the HERACLES Diagnostic Criteria validation study, two (with A0485) and one (with Pathway) of 17 ISH-amplified cases showed 3+ staining in 10 to 30 percent of cells.2 In another recent study by Shimada, et al., among 201 colorectal cancers, 10 tumors (five percent) showed 3+ staining in ≥50 percent of cells, while two tumors (one percent) showed 3+ staining in ≥10 percent but <50 percent of cells.12 Thus, if one decides to perform ISH on cases showing IHC 3+ staining in the 10 to 50 percent range, it would not appear overly burdensome (i.e. HER2 overexpression in colorectal cancer appears to be less heterogeneous than in gastroesophageal adenocarcinoma). Given less apparent heterogeneity in colon cancer and lack of clinical validation, I do not use the separate HER2 IHC biopsy criteria employed in gastroesophageal adenocarcinomas.
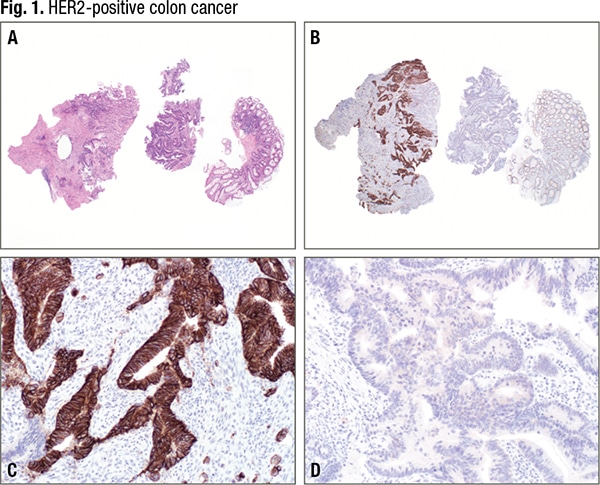
A 63-year-old man presented with six months of change in bowel habits and 25-pound weight loss. Colonoscopy demonstrated a circumferential rectal mass, with biopsy showing adenocarcinoma (A). Imaging highlighted metastatic disease in the lungs, liver, and L2 vertebral body. The tumor was RAS/RAF wild type and showed proficient DNA mismatch repair status. HER2 amplification was identified on circulating tumor DNA testing, which medical oncology asked us to confirm in the tissue. HER2 immunostain (B) demonstrates areas of strong, basolateral-predominant staining (C) and absent staining (D). Overall, 50 percent of the tumor was HER2 overexpressing. The patient was initially treated with FOLFOX, to which bevacizumab was added for the third cycle. The tumor initially responded and the patient was transitioned to capecitabine plus bevacizumab maintenance therapy. The patient was switched to FOLFIRI plus panitumumab on disease progression. The tumor progressed on this therapy, and the patient, now 16 months from initial diagnosis, was recently begun on trastuzumab and lapatinib.
In addition to consternation about scoring criteria, I receive questions about what tissue to test. In colon cancer in general, there is a high concordance for oncogenic driver mutations in matched primary-metastatic pairs. Brannon, et al., recently reported 100 percent concordance for KRAS, NRAS, and BRAF mutations in 69 matched primary-metastatic tumors.13 Regarding HER2 specifically, in the HERACLES validation study, there was 100 percent concordance in matched primary-metastatic pairs when assessed by Pathway and ISH (3+ or amplified in primary and metastasis in four of 47 patients).2 Similarly, in the Shimada, et al., study, among 45 matched primary-metastatic pairs, both tumors were IHC positive in three, both were IHC negative in 41, and one tumor was positive in the primary and negative in the metastasis.12 In a retrospective analysis of material from 3,256 colon cancer patients enrolled in three large clinical trials, Richman, et al., found HER2 overexpression to be more common in stage IV (2.2 percent; 29/1,342 patients) than stage II–III disease (1.3 percent; 25/1,914).14 HER2 overexpression leads to RAS/RAF/MAPK and PI3K/AKT pathway activation, and, like KRAS mutations (and other molecular genetic events in these signaling pathways), HER2 positivity has been shown to confer resistance to anti-EGFR therapy in both the preclinical and clinical settings.15-18 HER2 positivity is much more common in KRAS wild-type tumors (and is probably also largely mutually exclusive of NRAS and BRAF activating mutations).13,15 Richman, et al., found HER2 overexpression in 5.2 percent of KRAS wild-type and only one percent of KRAS mutant tumors.14 Similarly, in the initial portion of the HERACLES validation, Valtorta, et al., found HER2 positivity in 0/44 (zero percent) KRAS mutant and 17/304 (5.6 percent) KRAS wild-type tumors. Finally, though there is little data to date, acquisition of HER2 positivity has been reported as a mechanism for acquired cetuximab resistance.19
Taken all together, HER2 testing may be useful in the metastatic setting, especially if anti-EGFR therapy is being contemplated. Testing of either primary or metastatic tumor appears appropriate, with the consideration that HER2 activation may arise de novo in the setting of anti-EGFR therapy. At this point, I only perform HER2 testing in colon cancer at medical oncology’s request (Fig. 1). Sometimes this is to confirm HER2 amplification detected on next-generation sequencing of tumor or circulating tumor DNA. According to NCCN guidelines, in patients appropriate for intensive therapy, dual anti-HER2 therapy is an option only in HER2-positive patients with advanced disease who have progressed on at least one line of standard therapy; in version 1 of the 2020 guidelines, dual anti-HER2 therapy was added as an option for first-line therapy in HER2-positive patients with advanced disease who are not appropriate for intensive therapy.20 The activity of this therapy compares favorably to regorafenib and trifluridine plus tipiracil.
Although most well known in breast and gastroesophageal adenocarcinomas, HER2 activation occurs in diverse carcinoma types, as highlighted by results of recent Cancer Genome Atlas studies (Fig. 2). Anti-HER2 therapies have been examined in clinical trials of non-breast/non-gastroesophageal carcinomas for 20 years but appear to be gaining significant traction. Earlier trials were often characterized by inferior patient selection (e.g. not biomarker driven or inclusion of IHC 2+), single-agent therapy, and poor accrual. In addition to activity in colorectal cancer, the MyPathway trial has also reported signal in small cohorts of salivary gland, pancreatobiliary, bladder, non-small cell lung, and ovarian cancers,21 and addition of trastuzumab to carboplatin-paclitaxel improved progression-free survival in a separate phase two trial of uterine serous carcinoma.22 Ado-trastuzumab emtansine (trastuzumab covalently bound to the cytotoxic microtubule inhibitor DM1) showed activity in HER2-mutant lung adenocarcinoma (no screened, eligible patients were HER2 IHC 3+)23; in another cohort from the same basket trial, nine of 10 HER2-amplified salivary gland carcinoma patients achieved an objective response, including five complete responders.24

Given these positive clinical trial results, pathologists may increasingly face requests for HER2 testing in diverse solid tumors. At present, I report the intensity (0–3+, based on the magnification rule) and extent (0–100 percent) of lateral membrane, basolateral, or complete membrane staining. I reflexively FISH cases at the IHC 2+, ≥10 percent cells staining threshold. To satisfy CAP requirements regarding predictive marker reporting (ANP.22969 Report Elements), I have composed the following templated language for HER2 IHC (and analogous language for HER2 ISH):
HER2 immunohistochemistry is performed on formalin-fixed, paraffin-embedded tissue sections from non-breast/non-gastroesophageal carcinoma tissue using the rabbit monoclonal antibody SP3 and a polymer-based detection system.
There are no uniformly agreed on criteria in these tumor types. Recent clinical trials of anti-HER2 therapy have employed different selection criteria. Anti-HER2 therapy is currently only FDA approved in breast and gastric/gastroesophageal junction carcinomas.
MyPathway is a multiple basket trial that has enrolled patients with diverse solid tumors for dual anti-HER2 therapy based on HER2 activation detected by IHC, ISH, or NGS. IHC criteria were borrowed from breast, with the caveat that lateral membrane and basolateral staining were also considered. There are no separate biopsy criteria:
Score 0: No staining or membrane staining in <10% of tumor cells.
Score 1+: Membrane staining in ≥10% of tumor cells of faint/barely perceptible intensity.
Score 2+: Complete, basolateral, or lateral membrane staining in ≥10% of tumor cells of weak to moderate intensity.
Score 3+: Complete, basolateral, or lateral membrane staining in ≥10% of tumor cells of strong intensity.
Hainsworth JD, Meric-Bernstam F, Swanton C, Hurwitz H, Spigel DR, Sweeney C, et al. Targeted therapy for advanced solid tumors on the basis of molecular profiles: results from MyPathway, an open-label, phase IIa multiple basket study. J Clin Oncol.2018;36(6):536–542.
-
- Sartore-Bianchi A, Trusolino L, Martino C, et al. Dual-targeted therapy with trastuzumab and lapatinib in treatment-refractory, KRAS codon 12/13 wild-type, HER2-positive metastatic colorectal cancer (HERACLES): a proof-of-concept, multicentre, open-label, phase 2 trial. Lancet Oncol. 2016;17(6):738–746.
- Valtorta E, Martino C, Sartore-Bianchi A, et al. Assessment of a HER2 scoring system for colorectal cancer: results from a validation study. Mod Pathol. 2015;28(11):1481–1491.
- Meric-Bernstam F, Hurwitz H, Raghav KPS, et al. Pertuzumab plus trastuzumab for HER2-amplified metastatic colorectal cancer (MyPathway): an updated report from a multicentre, open-label, phase 2a, multiple basket study. Lancet Oncol. 2019;20(4):518–530.
- Rüschoff J, Dietel M, Baretton G, et al. HER2 diagnostics in gastric cancer-guideline validation and development of standardized immunohistochemical testing. Virchows Arch. 2010;457(3):299–307.
- Siena S, Sartore-Bianchi A, Marsoni S, et al. Targeting the human epidermal growth factor receptor 2 (HER2) oncogene in colorectal cancer. Ann Oncol. 2018;29(5):1108–1119.
- Rüschoff J, Hanna W, Bilous M, et al. HER2 testing in gastric cancer: a practical approach. Mod Pathol. 2012;25(5):637–650.
- Hofmann M, Stoss O, Shi D, et al. Assessment of a HER2 scoring system for gastric cancer: results from a validation study. Histopathology. 2008;52(7):797–805.
- Bartley AN, Washington MK, Ventura CB, et al. HER2 testing and clinical decision making in gastroesophageal adenocarcinoma: guideline from the College of American Pathologists, American Society for Clinical Pathology, and American Society of Clinical Oncology. Arch Pathol Lab Med. 2016;140(12):1345-1363.
- Atkinson R, Mollerup J, Laenkholm AV, et al. Effects of the change in cutoff values for human epidermal growth factor receptor 2 status by immunohistochemistry and fluorescence in situ hybridization: a study comparing conventional brightfield microscopy, image analysis-assisted microscopy, and interobserver variation. Arch Pathol Lab Med. 2011;135(8):1010–1016.
- Zhang X, Bleiweiss I, Jaffer S, Nayak A. The impact of 2013 updated ASCO/CAP HER2 guidelines on the diagnosis and management of invasive breast cancer: a single-center study of 1739 cases. Clin Breast Cancer. 2017;17(6):486–492.
- Lim TH, Lim AS, Thike AA, Tien SL, Tan PH. Implications of the updated 2013 American Society of Clinical Oncology/College of American Pathologists guideline recommendations on human epidermal growth factor receptor 2 gene testing using immunohistochemistry and fluorescence in situ hybridization for breast cancer. Arch Pathol Lab Med. 2016;140(2):140–147.
- Shimada Y, Yagi R, Kameyama H, et al. Utility of comprehensive genomic sequencing for detecting HER2-positive colorectal cancer. Hum Pathol. 2017;66:1–9.
- Brannon AR, Vakiani E, Sylvester BE, et al. Comparative sequencing analysis reveals high genomic concordance between matched primary and metastatic colorectal cancer lesions. Genome Biol. 2014;15(8):454.
- Richman SD, Southward K, Chambers P, et al. HER2 overexpression and amplification as a potential therapeutic target in colorectal cancer: analysis of 3256 patients enrolled in the QUASAR, FOCUS and PICCOLO colorectal cancer trials. J Pathol. 2016;238(4):562–570.
- Bertotti A, Papp E, Jones S, et al. The genomic landscape of response to EGFR blockade in colorectal cancer. Nature. 2015;526(7572):263–267.
- Kavuri SM, Jain N, Galimi F, et al. HER2 activating mutations are targets for colorectal cancer treatment. Cancer Discov. 2015;5(8):832–841.
- Martin V, Landi L, Molinari F, et al. HER2 gene copy number status may influence clinical efficacy to anti-EGFR monoclonal antibodies in metastatic colorectal cancer patients. Br J Cancer. 2013;108(3):668–675.
- Sartore-Bianchi A, Amatu A, Porcu L, et al. HER2 positivity predicts unresponsiveness to EGFR-targeted treatment in metastatic colorectal cancer. Oncologist. 2019;24(10):1395–1402.
- Takegawa N, Yonesaka K, Sakai K, et al. HER2 genomic amplification in circulating tumor DNA from patients with cetuximab-resistant colorectal cancer. Oncotarget. 2016;7(3):3453–3460.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Colon Cancer. Version 1.2020. https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf.
- Hainsworth JD, Meric-Bernstam F, Swanton C, et al. Targeted therapy for advanced solid tumors on the basis of molecular profiles: results from MyPathway, an open-label, phase IIa multiple basket study. J Clin Oncol. 2018;36(6):536–542.
- Fader AN, Roque DM, Siegel E, et al. Randomized phase II trial of carboplatin-paclitaxel versus carboplatin-paclitaxel-trastuzumab in uterine serous carcinomas that overexpress human epidermal growth factor receptor 2/neu. J Clin Oncol. 2018;36(20):2044–2051.
- Li BT, Shen R, Buonocore D, et al. Ado-trastuzumab emtansine for patients with HER2-mutant lung cancers: results from a phase II basket trial. J Clin Oncol. 2018;36(24):2532–2537.
- Li BT, Shen R, Offin M, et al. Ado-trastuzumab emtansine in patients with HER2 amplified salivary gland cancers (SGCs): results from a phase II basket trial. J Clin Oncol. 2019;37(suppl 15):6001.
Andrew Michael Bellizzi, MD
Clinical Associate Professor
Department of Pathology
University of Iowa Hospitals and Clinics
Director of Immunohistochemistry
Director of GI Pathology
Holden Comprehensive Cancer Center
Iowa City, Iowa
Chair, CAP Immunohistochemistry Committee