Editor: Frederick L. Kiechle, MD, PhD
Submit your pathology-related question for reply by appropriate medical consultants. CAP TODAY will make every effort to answer all relevant questions. However, those questions that are not of general interest may not receive a reply. For your question to be considered, you must include your name and address; this information will be omitted if your question is published in CAP TODAY.
Q. A semen analysis for viability was collected at 9:30 AM and not received in the laboratory until 1:40 PM. Our standard operating procedure says this test must be analyzed one hour after collection, with no disclaimers stated for late receivables. Therefore, it is my understanding that a specimen received five hours after collection would be considered unacceptable because the viability of the semen is compromised and the collection delivery does not follow our SOP. My supervisor advised accepting the specimen and putting a disclaimer on it: “The receipt time in lab was 1:40 PM. Test may be compromised.” This is not in the SOP. I feel this specimen should have been rejected and re-collected. This is not the first time this has occurred. Laboratory technicians put their name on the test with the disclaimer, not the supervisor.
A. The first issue is the laboratory has an SOP that states semen specimens “must be analyzed one hour after collection.” The specimen was collected at 9:30 AM and received at the lab at 1:40 PM. To test and report the specimen would be a deviation from the SOP. In short, the lab did not follow its standard operating procedure.
Second, it appears the lab is not following the current recommendations for semen analysis regarding sample collection. Per the WHO Laboratory Manual for the Examination and Processing of Human Semen, 5th ed., sections 2.2.5 and 2.2.6 recommend the semen sample be delivered to the laboratory within one hour of collection.
Third, the SOP should be updated to specifically address what to do in the event the specimen arrives in the laboratory outside of the allowable testing period.
Last, to help reduce the number of samples received out of stability, the lab should consider preparing an informational sheet or pamphlet to give to the patient that describes the allowable collection methods and time frame for return of the specimen to the laboratory. All aspects of semen analysis, including collection, should be standardized if the results are to provide valid, useful information.
World Health Organization. WHO Laboratory Manual for the Examination and Processing of Human Semen, 5th ed. Geneva: WHO Press; 2010.
Robert Saunders McGee Jr., MD, PhD
Medical Director, Global Anatomic Pathology/Histology
Covance Central Laboratory Services
Indianapolis
Member, CAP Reproductive Medicine Committee
Q. What is the PD-L1 immunohistochemistry combined positive score and how does it compare with the tumor proportion score?
A. On Sept. 22, 2017 the Food and Drug Administration granted accelerated approval to pembrolizumab (Keytruda) for patients with recurrent locally advanced or metastatic gastric or gastroesophageal junction adenocarcinoma whose tumors express PD-L1 as determined by an FDA-approved test.1
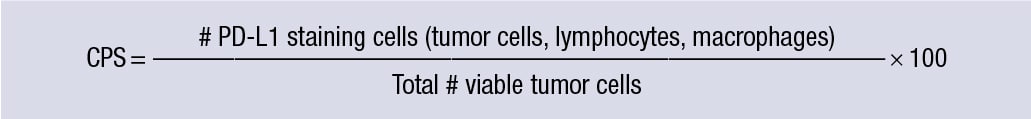 The approval was based on results of a phase two study (Keynote-059) that enrolled 259 patients with gastric or GEJ adenocarcinoma and showed an improved objective response rate in patients with tumors expressing PD-L1.2,3 The FDA-approved PD-L1 test used in this study was the PD-L1 22C3 pharmDx (Dako) using the following combined positive score (CPS) formula, with PD-L1 expression defined as a CPS ≥ 1.
The approval was based on results of a phase two study (Keynote-059) that enrolled 259 patients with gastric or GEJ adenocarcinoma and showed an improved objective response rate in patients with tumors expressing PD-L1.2,3 The FDA-approved PD-L1 test used in this study was the PD-L1 22C3 pharmDx (Dako) using the following combined positive score (CPS) formula, with PD-L1 expression defined as a CPS ≥ 1.
CPS is distinct from TPS. Both the combined positive score and the tumor proportion score (TPS) are FDA-approved IHC scoring systems for PD-L1 expression. However, the two scores apply to two different tumor types: CPS is used for gastric or GEJ adenocarcinoma, whereas TPS is used for non-small cell lung cancer. Additionally, TPS is defined as the percentage of viable tumor cells showing partial or complete membrane staining at any intensity; it does not consider staining in non-tumor cells.
The CPS numerator. The cell types included in the CPS numerator are tumor cells as well as tumor-associated lymphocytes and macrophages. All other cell types are excluded, including plasma cells, eosinophils, and neutrophils.
Staining is best assessed at 20× magnification. For tumor cells, analogous to the approach for the TPS in lung cancer, any convincing partial or complete linear membrane staining (≥ 1+) is considered as PD-L1 staining. Cytoplasmic staining alone in tumor cells is not regarded as positive. The scoring for macrophages is similar to that for tumor cells. For lymphocytes, however, the positively stained cells tend to have indistinguishable membranous and cytoplasmic staining owing to these cells’ high nucleus to cytoplasm ratio; as such, both membranous and cytoplasmic staining (≥ 1+) are considered positive.3
The CPS denominator. Only viable tumor cells are included in the CPS denominator. A minimum of 100 tumor cells must be present in the PD-L1-stained slide (biopsy or resection) for the specimen to be considered adequate for evaluation.
The maximum score for CPS. Although the result of the CPS calculation can exceed 100, the maximum score is defined as CPS 100.3
 Scoring heterogeneously stained samples. The general recommendation for scoring the CPS is that it be performed within the context of the pathologist’s past experience and best judgment in interpreting IHC stains. In cases where the staining is patchy, one may base the scoring on the area or areas that have the highest number of both positively stained cells (per the CPS numerator) and viable tumor cells. In cases where only one area shows positive staining, that area would constitute the basis for the CPS. In cases where different regions show positivity, the average of the combined positive scores from these different regions may be used. If a case shows only a few scattered positively stained cells, then the numerator would be the total number of the positive cells (per the CPS numerator), and the denominator would be the total number of the tumor cells within the area that the positive cells span.
Scoring heterogeneously stained samples. The general recommendation for scoring the CPS is that it be performed within the context of the pathologist’s past experience and best judgment in interpreting IHC stains. In cases where the staining is patchy, one may base the scoring on the area or areas that have the highest number of both positively stained cells (per the CPS numerator) and viable tumor cells. In cases where only one area shows positive staining, that area would constitute the basis for the CPS. In cases where different regions show positivity, the average of the combined positive scores from these different regions may be used. If a case shows only a few scattered positively stained cells, then the numerator would be the total number of the positive cells (per the CPS numerator), and the denominator would be the total number of the tumor cells within the area that the positive cells span.
PD-L1 IHC 22C3 pharmDx versus other clones. The FDA-approved PD-L1 IHC test in this clinical setting is the Dako 22C3 pharmDx. However, various other PD-L1 antibody clones exist, including 405.9A11; B7-H1; PD-L1, 5H1; SP263; SP142; 130021; 28-8; and E1L3N. Some institutions have validated the E1L3N clone from Cell Signaling Technology against the PD-L1 22C3 pharmDx and applied it to clinical cases.
Reporting. Although a CPS ≥ 1 would meet the FDA-approved PD-L1 IHC criterion for use of pembrolizumab in gastric and GEJ adenocarcinoma, as with other predictive markers, we recommend the actual score be indicated in the pathology report. Our institution also reports the relative contribution to the CPS by tumor cells versus immune cells (lymphocytes and macrophages). An example reporting format is as follows:
Summary. The CPS is a measure of PD-L1 positivity in both tumor cells and tumor-associated immune cells used in gastric and GEJ adenocarcinoma. The inclusion of immune cells distinguishes it from the TPS, another PD-L1 scoring system used in lung cancers. Accurate evaluation of the CPS hinges on a thorough understanding of how positivity is defined and what cellular components are to be analyzed.
- U.S. Food and Drug Administration. FDA grants accelerated approval to pembrolizumab for advanced gastric cancer. https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm577093.htm. Updated Sept. 22, 2017.
- Fuchs CS, Doi T, Jang RW-J, et al. KEYNOTE-059 cohort 1: efficacy and safety of pembrolizumab (pembro) monotherapy in patients with previously treated advanced gastric cancer. J Clin Oncol. 2017;35(15 suppl):4003.
- PD-L1 IHC 22C3 pharmDx Interpretation Manual—Gastric or Gastroesophageal Junction (GEJ) Adenocarcinoma. Carpinteria, Calif.: Dako, Agilent Pathology Solutions; 2017. www.bit.ly/22C3pharmDx_manual.
Jinru Shia, MD
Attending Pathologist, Memorial Sloan Kettering Cancer Center
Professor of Pathology and Laboratory Medicine
Weill Cornell Medical College, New York, NY
Member, CAP Immunohistochemistry Committee