Editor: Frederick L. Kiechle, MD, PhD
Submit your pathology-related question for reply by appropriate medical consultants. CAP TODAY will make every effort to answer all relevant questions. However, those questions that are not of general interest may not receive a reply. For your question to be considered, you must include your name and address; this information will be omitted if your question is published in CAP TODAY.
Q. Is there clinical value in doing routine manual band counts to detect infection in newborns, especially since procalcitonin and immature neutrophil counts are available?
A. September 2019—Instrument-generated automated differential counts combine bands and neutrophils in the single category of absolute neutrophil count (ANC). Enumeration of bands thus requires a manual differential. It is well recognized that enumeration of bands is problematic due to poor precision, small sample size, and interobserver variability.1,2 Moreover, it is insensitive, inefficient, and expensive, and it increases turnaround times. For these reasons, many laboratories have stopped making enumeration of bands a distinct category.
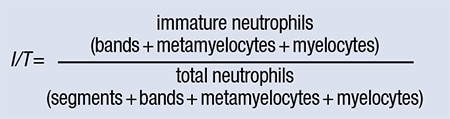
Historically, however, enumeration of bands has been used as a marker of left shift and an indicator of bacterial infection. There are several sepsis screening tools used clinically (see the Surviving Sepsis Campaign website for a partial listing, www.bit.ly/SepsisResources), and while many of the algorithms do not include band percentage as an evaluation criteria, some do. In adults and children older than three months, the white blood cell count and ANC are generally considered better indicators of infection than bandemia.3 In neonatal sepsis evaluation, the immature/total neutrophils (I/T) ratio continues to be used as one of the CBC parameters used clinically. The I/T ratio requires enumeration of bands (see formula below), with an I/T ratio of less than 0.2 being unlikely to have sepsis.
Multiple studies have evaluated the diagnostic value of CBC parameters in neonatal sepsis. While CBC abnormalities such as low white blood cell count, low ANC, and high I/T ratio were associated with culture-positive infections, no CBC-derived index is sufficiently sensitive. A high proportion of culture-negative babies (25–50 percent) may have a high I/T ratio. In most studies, the negative predictive value is higher, with a normal I/T ratio being more helpful in ruling out sepsis, although exhaustion of marrow reserves in critical illnesses can lead to false-negatives.
Several modern CBC analyzers offer a six-part differential, including a category of immature granulocytes (IG). Automated IGs include metamyelocytes, myelocytes, and promyelocytes but do not include bands. Since automation allows better precision and faster turnaround time, assessing left shift using automated IG enumeration, rather than a manual differential, is desirable. A large study evaluated more than 10,000 samples and concluded “that as a way to quantify the leukocyte ‘left shift’ the IG% and IG per μl from an automated differential count on the Sysmex hematology analyzer are comparable to the I/T ratio and absolute band count based on a manual differential count.”4
 Several studies have evaluated automated immature granulocyte counts and have found them to be of some utility in sepsis assessment.5,6 The utility of immature granulocytes in neonatal sepsis has also been evaluated in a few studies.7,8 Overall, both I/T ratio (and thus manual band counts) and automated IG have some utility in neonatal sepsis assessment, but both lack sufficient sensitivity. Automated IGs, however, offer the advantage of better precision, turnaround times, and cost. Given these considerations, if a laboratory wishes to replace manual band counting with automated IG reporting, a dialogue with the neonatologists is advised.
Several studies have evaluated automated immature granulocyte counts and have found them to be of some utility in sepsis assessment.5,6 The utility of immature granulocytes in neonatal sepsis has also been evaluated in a few studies.7,8 Overall, both I/T ratio (and thus manual band counts) and automated IG have some utility in neonatal sepsis assessment, but both lack sufficient sensitivity. Automated IGs, however, offer the advantage of better precision, turnaround times, and cost. Given these considerations, if a laboratory wishes to replace manual band counting with automated IG reporting, a dialogue with the neonatologists is advised.
A limited number of studies have evaluated other chemical markers of inflammation, including procalcitonin. Per Memar, et al., “Despite the promising data for some immunologic biomarkers, present evidence shows that none of them can constantly diagnose 100% of infections. IL-6 is the most potent marker for evaluation of EOS [early onset neonatal sepsis] prognosis. Procalcitonin (PCT) and C-reactive protein (CRP) are appropriate indicators for the detection and monitoring of antibiotics therapy.”9 A recently published review article suggested that serial measurements of C-reactive protein and other acute-phase reactants may be useful, with a lack of serial abnormalities supporting discontinuation of antibiotic therapy.10
- To and fro on band count reporting and clinical utility. CAP TODAY. 2010;24(11):54–60.
- Bhargava P, Nakashima MO. Q&A column. CAP TODAY. 2017;31(3):58–59.
- Cornbleet PJ. Clinical utility of the band count. Clin Lab Med. 2002;22(1):101–136.
- MacQueen BC, Christensen RD, Yoder BA, et al. Comparing automated vs manual leukocyte differential counts for quantifying the ‘left shift’ in the blood of neonates. Perinatol. 2016;36(10):843–848.
- Nierhaus A, Klatte S, Linssen J, et al. Revisiting the white blood cell count: immature granulocytes count as a diagnostic marker to discriminate between SIRS and sepsis—a prospective, observational study. BMC Immunol. 2013;14:8. doi:10.1186/1471-2172-14-8.
- van der Geest PJ, Mohseni M, Brouwer R, van der Hoven B, Steyerberg EW, Groeneveld AB. Immature granulocytes predict microbial infection and its adverse sequelae in the intensive care unit. J Crit Care. 2014;29(4):523–527.
- Cimenti C, Erwa W, Herkner KR, Kasper DC, Müller W, Resch B. The predictive value of immature granulocyte count and immature myeloid information in the diagnosis of neonatal sepsis. Clin Chem Lab Med. 2012;50(8):1429–1432.
- Nigro KG, O’Riordan M, Molloy EJ, Walsh MC, Sandhaus LM. Performance of an automated immature granulocyte count as a predictor of neonatal sepsis. Am J Clin Pathol. 2005;123(4):618–624.
- Memar MY, Alizadeh N, Varshochi M, Kafil HS. Immunologic biomarkers for diagnostic of early-onset neonatal sepsis. J Matern Fetal Neonatal Med. 2019;32(1):143–153.
- Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet. 2017;390(10104):1770–1780.
Parul Bhargava, MD
Professor of Clinical Laboratory Medicine
Director of Clinical Laboratories
Moffitt-Long Hospital
University of California San Francisco
Member, CAP Hematology/Clinical
Microscopy Committee
 In this “Best of Q&A” series, we reprint select coagulation-related questions and answers. All have been chosen for their timeliness and relevance today. The following question and answer were published in January 2014.
In this “Best of Q&A” series, we reprint select coagulation-related questions and answers. All have been chosen for their timeliness and relevance today. The following question and answer were published in January 2014.
Q. Patients who take statins may deplete their levels of CoQ10 (coenzyme Q10), and therefore many of these patients are now taking CoQ10 supplements. Can CoQ10 supplements affect the level of Coumadin (that is, the INR)?
A. Statins, commonly used to treat hypercholesterolemia, can cause myalgia. There have been suggestions that statins cause muscle injury by lowering levels of coenzyme Q10, which has a key role in mitochondrial respiration. The literature is sparse and the results are mixed regarding the ability of CoQ10 administration to reduce muscle symptoms. Nevertheless, patients may choose to take CoQ10 as a dietary supplement in an attempt to reduce myalgia caused by statins. Supplementation of CoQ10 has also been studied in heart failure and numerous other health conditions, but, again, a clear role for replacement has not been defined.
The interaction of warfarin with food, drugs, and some herbal products has been well recognized. In a systematic overview of publications related to warfarin interactions with drugs, food, and supplements,1 there were 92 substances with a probable or highly probable level of evidence supporting the potentiation or inhibition of warfarin. However, few studies have focused on CoQ10 and warfarin interactions/INR interference. In an animal study, Zhou, et al.,2 suggested that the accelerated metabolism of warfarin enantiomers (S and R forms) with concurrent CoQ10 treatment accounts for the reduced anticoagulant effect of warfarin in rats. The authors speculated that a moderate increase in the total clearance of warfarin enantiomers could occur with coadministration of CoQ10 in humans.
There are a few case reports of decreased INR after CoQ10 ingestion in humans.3 However, there is only one well-designed, randomized, double-blind study in the literature evaluating CoQ10 and warfarin.4 A small group of patients on stable warfarin treatment for different indications participated in this crossover study. Subjects took CoQ10 (100 mg/day)/warfarin for four weeks, ginkgo biloba/warfarin for four weeks, and placebo/warfarin for four weeks. There was no significant difference in INR for each combination. The authors concluded there was no significant interference during the coadministration of warfarin and CoQ10 but remained cautious, recommending close monitoring of the INR in these patients.
In summary, the best available evidence suggests that CoQ10 does not affect INR in humans, but the results of this single randomized, double-blind study have not been confirmed in additional well-designed studies. Additionally, the dose and potency of CoQ10 supplements have not clearly been established, so it seems reasonable to closely monitor patients taking warfarin and CoQ10.
- Holbrook AM, Pereira JA, Labiris R, et al. Systematic overview of warfarin and its drug and food interactions. Arch Intern Med. 2005;165(10):1095–1106.
- Zhou Q, Zhou S, Chan E. Effect of coenzyme Q10 on warfarin hydroxylation in rat and human liver microsomes. Curr Drug Metab. 2005;6(2):67–81.
- Spigset O. Reduced effect of warfarin caused by ubidecarenone. Lancet. 1994;344 (8933):1372–1373.
- Engelsen J, Nielsen JD, Winther K. Effect of coenzyme Q10 and Ginkgo biloba on warfarin dosage in stable, long-term warfarin treated outpatients. A randomised, double blind, placebo crossover trial. Thromb Haemost. 2002;87(6):1075–1076.
Arnaud Drouin, MD
Currently Assistant Professor, Department of Medicine
Adjunct Assistant Professor in Hematopathology
Department of Pathology and Laboratory Medicine
Tulane University School of Medicine, New Orleans
Former member of the CAP Coagulation Resource Committee at time of original publication
Russell A. Higgins, MD
Currently Professor, Clinical Department of Pathology and Laboratory Medicine
University of Texas Health San Antonio
Medical Director, University Health System Pathology Services, San Antonio
Chair of the CAP Coagulation Resource Committee at time of original publication