Karen Titus
August 2014—A slow leak in a tire may not be all that interesting— until one is cruising down the highway at 75 m.p.h. Suddenly, that same leak becomes much more compelling.
Joseph Misdraji, MD, recalls a conversation he had at a meeting about pseudomyxoma peritonei that skirted a similar curve in the road. Approached by a pathologist who expressed a desire to collaborate with him, Dr. Misdraji suggested a study he was working on, looking at the significance of proximal margin involvement in low-grade appendiceal mucinous neoplasms, or LAMN.
The pathologist’s response was as unequivocal as a negative node. “I’m paraphrasing, but it was basically, ‘I’ll wait until you’re doing something more important,’” recalls Dr. Misdraji, associate pathologist, Massachusetts General Hospital, and associate professor of pathology, Harvard Medical School, Boston.
Dr. Misdraji laughs about that conversation—he harbors more curiosity than ill will about the response. Any topic can seem small “if you’re not dealing with it right now,” he says. “But one day when you are dealing with it, or it’s your appendix, then you’d like to know that there’s some data upon which to base a recommendation.”
![Those who question a conservative approach are making the assumption that a positive margin leaves tumor behind and increases risk of recurrence. Data from the study published in Archives suggest otherwise. Says Dr. Misdraji, above: “Even if you think that’s a shocking approach [to be conservative], that’s what the majority treatment approach is already.”](http://www.captodayonline.com/wordpress/wp-content/uploads/2014/08/Misdraji_Joseph.jpg)
Those who question a conservative approach are making the assumption that a positive margin leaves tumor behind and increases risk of recurrence. Data from the study published in Archives suggest otherwise. Says Dr. Misdraji, above: “Even if you think that’s a shocking approach [to be conservative], that’s what the majority treatment approach is already.”
Now, there is. That study, so easily dismissed at the meeting, was recently published in an early online release in Archives of Pathology & Laboratory Medicine (www.archivesofpathology.org/doi/abs/10.5858/arpa.2014-0246-OA).
The retrospective study is small— 16 cases—but intriguing. It is, say its authors, the first data assembled to look at the implications of a positive margin in patients with LAMN. Or, as Dr. Misdraji puts it, “How alarmist should a pathologist be?” Should pathologists urge additional surgery or therapy in such cases? Or is a more conservative approach valid?
The paper is an effort to replace perception with evidence, says lead author Thomas Arnason, MD, attending anatomical pathologist, Queen Elizabeth II Health Sciences Centre, and assistant professor of pathology, Dalhousie University, Halifax, Nova Scotia.
“I think there’s an assumption in pathology, in general, that when you have a positive margin, it mandates further resection,” with the thought that disease will recur or spread if it’s present at the margin, says Dr. Arnason.
With this paper, the authors are suggesting otherwise. “In our experience, there is no evidence that will happen,” says Dr. Arnason.
As the paper notes, appendiceal adenomas and LAMNs that are confined to the appendix are cured by appendectomy. But when patients have positive margins, they may undergo cecal resection to reduce risk (or perceived risk) of recurrence or dissemination.
And why not? When Dr. Arnason and colleagues delivered the paper as a platform presentation at the USCAP annual meeting in March, one pathologist audience member responded with some degree of astonishment. (The comments were strong enough, Dr. Misdraji says, that they were addressed in the final paper.) The consequences of the tumor recurring as pseudomyxoma peritonei were so dire, the listener said, that the authors weren’t justified in suggesting conservative treatment, especially since cecectomy is a minimal procedure.
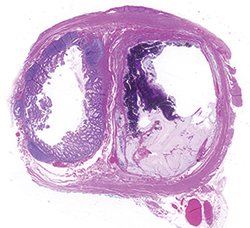
One challenge in the study was the classification of mucosal proliferations at the margin. This slide from the paper shows a case classified as dissecting mucin at the margin. The outside pathologists thought the epithelium lining the lumen of the appendix at the margin was neoplastic, while Dr. Misdraji and colleagues felt it was hyperplastic.
Dr. Arnason responds with Coolidge-like brevity: “It’s still surgery.” With it come small, but not zero, risks associated with anesthesia, bleeding, and infection, not to mention recovery time and cost.
Nor is there evidence to suggest that surgery is necessary. Proximal margin involvement in LAMNs has not been an area of intense research interest, as Dr. Misdraji’s would-be collaborator made clear. This is a little neck in a not-so-large woods. There’s been plenty written about mucinous tumors of the appendix that have spread throughout the abdomen as pseudomyxoma peritonei, says Dr. Misdraji, both in terms of their pathology and the need for aggressive treatment.
“Everybody knows what’s going on. It’s spread; it’s bad news.” Likewise, the literature does a fairly good job of addressing tumors that are confined to the appendix, the implications of which are similarly clear: Patients tend to do well, and their tumors are much more benign than those that have spread throughout the abdomen.
Dr. Misdraji rarely sees such straightforward cases in his role as a consultant. Instead, he receives queries involving tumors limited to the appendix but with positive margins: What does this mean?
In his reports, Dr. Misdraji would often rely on empirical evidence, noting that he’d never necessarily seen a recurrence in cases with a positive margin. “But then again, I’ve never done a sequential data collection to see what the data shows,” he says. He’d often recommend a conservative approach, such as a colonoscopy or radiographic study. “But again, I didn’t even have evidence upon which to base that.”
Eventually, he says, he felt he might be able to ask and answer the question with more rigor. Even with his broad consulting experience, however, it turned out to be surprisingly difficult to find cases appropriate for the study.

Dr. Arnason
“This is essentially a rare tumor,” says Dr. Arnason. Cases with a positive margin are even rarer, he adds, despite the experience compiled during Dr. Misdraji’s consults. Says Dr. Misdraji: “Even though I felt in my mind I had seen a lot of cases in consults, in fact, there were maybe only 10 cases.” As it turns out, finding cases proved to be the biggest challenge of the study. So Dr. Misdraji widened the search, turning to consult cases done by his predecessors at MGH as well as to the consult work of pathologists (and coauthors) Rhonda Yantiss, MD, of Weill Cornell Medical College, New York, NY, and Michelle Yang, MD, of the University of Massachusetts Memorial Medical Center, Worcester. Even with the combined experience of experts at multiple large hospitals, the yield was only those 16 cases (15 LAMNs, one adenoma).
The margins in these cases can be very subtle, says Dr. Misdraji, as the tumor itself is quite bland. At the same time, there can be hyperplastic changes in the mucosa at the margin. Judging margin involvement was a challenge—as illustrated by one of the photos published with the study. In this case (as in six others included in the study), there was no neoplastic epithelium at the margin, but there was dissecting acellular mucin. The case was included in the study because of the mucin dissection; though the original pathologists thought there was tumor at the margin, Dr. Misdraji and his coauthors thought it was merely hyperplastic. Such disagreements meant excluding other cases, in which “we were not convinced that it was clearly neoplastic epithelium at the margin,” Dr. Misdraji says. Cases that showed denuded mucosa at the margin or scant acellular mucin in the lumen were excluded, as were those with periappendiceal mucin, periappendiceal mucinous epithelium, or overtly malignant cytologic features.
This may represent a biological mystery in addition to being a research challenge. Dr. Misdraji says it’s possible that LAMN margins have their own peculiarities. Positive margins in pathology aren’t unknown—“They come across your desk every now and then,” as Dr. Misdraji puts it—and they certainly shouldn’t be absent in this particular situation, he says. “So what is it about the biology of the appendix at its orifice that’s different from the rest of the appendix? Why do these tumors tend to go more toward the middle or tip, or not involve or not spread into the cecum quite so easily?”
As played out in clinical practice, the question becomes, Why does an involved margin not recur in a subsequent resection? Perhaps as pathologists try to take a margin, says Dr. Misdraji, they may, not infrequently, encounter a staple (for example) that requires them to look at an adjacent section. In that scenario, “You’re not quite looking at the edge of the tissue. You’re probably looking at a sample of the edge. It’s the next best thing—something interpretable at that edge,” Dr. Misdraji says. It’s possible, he adds, that pathologists could interpret this as a “margin” even though it’s 1 or 2 mm from the actual margin.
Finally, the authors needed cases with adequate follow-up, though one pathologist’s “adequate” may be another’s “insufficient.” One case is listed as “recent,” while the other cases range in follow-up interval from one year to 11.7 years; mean follow-up was 4.7 years, and median follow-up was 3.5 years. “Some physicians who look at this study may say the follow-up period isn’t quite as long as we’d ideally like to see,” Dr. Arnason says. “For now, it’s the best we can do.”
Once the cases were all on the same page, so to speak, what did the researchers find?
Six patients underwent cecal resection; the other 10 were followed nonsurgically. No cecal resection had residual neoplasia, the authors write, and no patient developed recurrence or pseudomyxoma peritonei.
Dr. Misdraji says two things surprised him: one, that a large (relatively speaking) number of patients did not have surgical follow-up, and two, that findings were so consistent. Surely one or two patients might have had something in the resection specimen that would suggest a more aggressive treatment, he says. In fact, the vehement response from the aforementioned USCAP attendee was not an outlier. Pathologists are leery of LAMNs.
Dr. Misdraji has two responses. “Data is data,” he says. “I feel you can make your recommendations only based on data.” Those who question a conservative approach are making the assumption that a positive margin leaves tumor behind and increases risk of recurrence. But so far, he says, the data—his—suggest that’s not true.
Secondly, he says, “Even if you think that’s a shocking approach [to be conservative], that’s what the majority treatment approach is already. You may not agree with it, but apparently many surgeons seem to agree with it. They don’t do anything anyway.”
Why aren’t surgeons more aggressive? Neither Dr. Misdraji nor Dr. Arnason has yet had an opportunity to discuss their findings with their surgeon colleagues. Dr. Misdraji says he suspects many patients are told their disease is not aggressive. “I think surgeons maybe downplay its importance, or maybe correctly assess its importance,” with the result that they may not steer patients toward a cecectomy. “You don’t want to necessarily alarm the patient,” he says.
Despite their concerns about conservative follow-up, pathologists may not push those views, Dr. Misdraji continues. When pathologists note a positive margin, they’re unlikely to force a surgeon’s hand by urging additional surgery, he says. “They don’t tend to make bold or aggressive recommendations.” In some cases, he adds, there may be limited understanding of the lesion’s biology. Something signed out as a cystadenoma, even with a positive margin, “sounds so benign.” Likewise, something identified as a LAMN with a positive margin “still doesn’t sound like cancer, and they may not feel compelled to act despite hearing there’s an involved margin.”
Surgeons also weigh other factors when considering surgery—age, comorbidities, etc.—and may decide those risks outweigh that of recurrence, says Dr. Arnason. But he says some pathologists have responded to the study by telling him that regardless of the data, they’ll still likely recommend an additional resection. Assumptions die hard, he says, and concerns of theoretical risk remain.
What’s next? Longer follow-up would be helpful. There are no formal plans to track the patients in the study, but the possibility remains open. “We might revisit these people in five years,” Dr. Arnason says, noting that the disease is slow and progressive, and thus there’s a slight possibility that someone could recur.
More cases would also be welcome. Dr. Misdraji noted, in July, that he hadn’t seen a case since the “recent” one mentioned in the paper. The authors say they’re eager to add to that number; indeed, they’re hoping their paper will spur additional discussion or research. Dr. Misdraji says he wouldn’t be surprised if, postpublication, he hears from colleagues who say they have had cases of recurrence. “We certainly need more than these 16 cases,” he says, though the paper notes that the literature describes at least four other cases of low-grade appendiceal neoplasms with positive appendectomy margins with no additional tumor in resection specimens. “Cumulatively we need a bigger data set to be able to advise people who are in this predicament. Is surgery wise, or is it unnecessary?”
But 16 isn’t nothing. Literally. To those who point out 16 isn’t a huge number, Dr. Misdraji offers this rejoinder: “It’s more than zero.” And, he says, it’s more than anecdotal evidence. “We have to start somewhere.”
[hr]
Karen Titus is CAP TODAY contributing editor and co-managing editor.