Anne Ford
August 2015—It sounds a bit like an Agatha Christie story: Two hospital patients, two lengthy stays, two adjacent but separate rooms. Patient A comes in with a Klebsiella pneumoniae carbapenemase-producing isolate. Patient B doesn’t . . . but within 30 days, he’s acquired it. How?
That’s the question Romney Humphries, PhD, section chief of clinical microbiology in the Department of Pathology and Laboratory Medicine at UCLA Health System, found herself asking recently.
Just like the plot of a classic murder novel, her inquiry—which she discussed as part of “Superbugs on Medical Devices—The UCLA Experience,” a talk at this year’s American Society for Microbiology meeting—yielded additional mysteries, a couple of red herrings, an exciting conclusion, and a few tantalizing loose ends.
After learning in late 2014 of the possible patient-to-patient KPC transmission, Dr. Humphries turned to the Los Angeles County Department of Public Health laboratory, which performed pulsed-field gel electrophoresis strain typing on the isolates. “But it was fairly inconclusive, partly because all our carbapenem-resistant Klebsiella pneumoniae in the Los Angeles area are fairly similar, and so it was hard to really figure out what was going on,” she explained.
Two of UCLA Health’s clinical microbiology fellows, Shaun Yang, PhD, and Peera Hemarajata, PhD, then had the idea of trying whole genome sequencing. “So they pulled these two isolates out of our collection and did some DNA prep, and about the time they were getting ready to send the isolates off for sequencing, they were chatting with the infectious diseases service, who mentioned they had a new patient with a CRE,” Dr. Humphries said. Just for the heck of it, Drs. Yang and Hemarajata decided to test an isolate from that third patient as well.

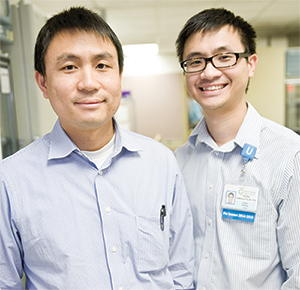
Dr. Romney Humphries: “The carbapenemase that was present was an OXA-232,” which had been reported only once before in the U.S. “We really didn’t expect to find this,” she says. Below: Microbiology fellows Dr. Shaun Yang (left) and Dr. Peera Hemarajata, whom Dr. Humphries credits for discovering the outbreak.
To no one’s surprise, the whole genome sequencing showed that the first two isolates were virtually indistinguishable. “I mean, this really was a patient-to-patient transmission based on the whole genome,” Dr. Humphries said. But what the whole genome sequencing revealed about the third isolate “blew our minds a little bit.”
That’s because the third isolate showed no KPC. “Instead, the carbapenemase that was present was an OXA-232. We really didn’t expect to find this.” As Dr. Humphries explained, OXA-232 is part of the OXA-48-like carbapenemase family. It had been reported only once previously in the United States, in a 2013 case in Pittsburgh.
 “So when we looked back at this patient, we expected to find some sort of travel history,” she continued. “She was a 48-year-old woman who had come in with cirrhosis of unknown etiology and had a liver transplant done at our center. Postoperative chest X-rays showed a plural effusion, and tracheal sections grew this Klebsiella that we then sequenced. Her transplant was unfortunately complicated by a bile leak; they went in and placed a stent via endoscopic retrograde cholangiopancreatography, or ERCP. Over the next several weeks, she developed sepsis and had an intra-abdominal infection and unfortunately died two months after her transplant—but surprisingly, she had absolutely no travel history that would explain her having this unusual Klebsiella.”
“So when we looked back at this patient, we expected to find some sort of travel history,” she continued. “She was a 48-year-old woman who had come in with cirrhosis of unknown etiology and had a liver transplant done at our center. Postoperative chest X-rays showed a plural effusion, and tracheal sections grew this Klebsiella that we then sequenced. Her transplant was unfortunately complicated by a bile leak; they went in and placed a stent via endoscopic retrograde cholangiopancreatography, or ERCP. Over the next several weeks, she developed sepsis and had an intra-abdominal infection and unfortunately died two months after her transplant—but surprisingly, she had absolutely no travel history that would explain her having this unusual Klebsiella.”
After briefly considering, then dismissing as highly unlikely, the possibility that the woman had somehow acquired Klebsiella from the liver donor, Dr. Humphries and her team asked themselves: Was this the first instance of OXA-232 at UCLA, or not?
“One of the interesting things about this isolate,” she told the audience, “is that it tested negative by our carbapenemase PCR that we perform for epidemiological purposes, and this is supposed to include the OXA-48-like carbapenemase family. But when we went back and looked at the former primer, of course there were a couple of mismatches in it that resulted in the inability to detect OXA-232 or OXA-181, which is very close; it only has the one base pair mutation that differentiates it from OXA-232.”
Upon going back and looking at its collection, the team again saw that the vast number of isolates were KPCs. “But there still remained this group of isolates for which we didn’t know the mechanism for carbapenem resistance,” Dr. Humphries pointed out. Were they all perhaps OXA-232s? Had this been a problem of longstanding duration at UCLA, without anyone realizing it?
She theorized that perhaps this was something of which she wasn’t aware that had been found in the Los Angeles area. But the CDC had no reports of OXA-232 other than the one from Pittsburgh. “So we designed a new PCR, kind of on the fly, so we could start looking for this,” she said. Dr. Hemarajata came up with a PCR to specifically look for a single base pair mutation, an A to a T, that would allow the user to differentiate an OXA-232 enzyme from an OXA-181.
“Essentially how this works is, you have your typical forward and reverse PCR, but you have excess of your reverse primer, so you end up with lots of the reverse strand,” Dr. Humphries explained. “And you have a probe that’s homologous to that reverse strand, and then you do high-resolution melt. And so what you find is, you get a melt when your probe is coming off and then a melt for your PCR product, allowing differentiation of OXA-181/232 from other OXA-48-like, and specific differentiation of OXA-232 from OXA-181.”
Thankful that they had stocked all carbapenem-resistant Enterobacteriaceae since 2010, Dr. Humphries’ team went back and tested everything from 2010 to 2013 that had been called carbapenemase-negative, and found they were all negative for OXA-232.
“And then we went ahead and tested all isolates from 2014,” she said, “and it just so happened that the isolate we did whole genome sequencing on was the first OXA-232 that we had seen at UCLA. Talk about luck, right?”
As Drs. Yang and Hemarajata began prospectively screening all CRE, cases began popping up all over the place. “We had a total of eight patients who had 25 of these isolates,” Dr. Humphries reported. “They were patients across six different units. They were mostly adults, but there was a handful of pediatrics in there, too.
“And the common factor was they had all had this endoscopic retrograde cholangiopancreatography procedure done before we isolated the OXA-232, with the exception of that first patient that we had done full genome sequencing on, who had her ERCP done after we isolated the organism.” Aha!
When reviewing epidemiology of CRE-infected patients before they knew this, they couldn’t identify ERCP as the risk factor for CRE infection at their institution. “But when we knew what the mechanism for resistance was,” she said, “it became very clear that this is where this was coming from. So I think it speaks to how important it is to be able to do some sort of genotype testing, especially if you are seeing an increase of CRE at your institution, to figure out what’s going on.”
What was going on in this case: After use, endoscopes were being cleaned and disinfected—but not well enough. “The ERCP scopes and the endoscopic ultrasound scopes have an elevator channel. This is like a hinge mechanism that allows for manipulations during the procedure, but it’s very, very difficult to get into these nooks and crannies and actually clean these elevator mechanisms,” Dr. Humphries said. “So you can imagine that if people are not very, very diligent about the cleaning and high-level disinfection between patients, it’s easy for small numbers of bacteria to remain present.”
At the time, UCLA Health had eight ERCP scopes. All eight patients involved in the outbreak had been exposed to one of two of them, and all eight patients had identical OXA-232 strands of Klebsiella pneumoniae.
Immediately, UCLA stopped all ERCP procedures, reported the outbreak to the Los Angeles County Department of Health, and cultured the scopes—twice. “We did it once using our lab-developed method, and then a second time using the draft guidance that was put out by the CDC, and it was negative in both cases,” she said. “And we did PCR off of those specimens for this OXA-232 gene, and that was also negative. And we also looked at the ATP levels on the scopes, and they were less than 100 units for both of the endoscopes.” Neither UCLA nor any outside entity was able to identify deficiencies in the scope-disinfection process that could explain the outbreak.
The team began sending out all ERCP duodenoscopes, as well as the endoscopic ultrasound scopes, for ethylene oxide sterilization after every single use. “Since we started doing that, we haven’t had a single OXA-232 case at our institution,” said Dr. Humphries. “So this pretty much put an end to our CRE problem.” It did, however, increase the scope reprocessing time significantly, requiring the number of scopes to be doubled. It also resulted in significant sterilization costs.
Then, too, “We’ve been doing this for a couple of months now, and our scopes have become very brittle,” she said. “It’s really hard on the scopes when you do it every time. They’re not designed for this. And there’s a lot of safety concerns, to be honest, that we have about using ethylene oxide. Ethylene oxide enteritis is a known entity for patients if a scope is not adequately de-gassed.” There’s concern also for the safety of the technicians who are providing the ethylene oxide treatments. “And it’s not available in many hospitals. We’re lucky we’re in Los Angeles, and so there’s a place in town that can do this for us, but obviously that’s not a solution for everyone.”
Added Dr. Humphries: “Probably a redesign of these scopes is needed. ERCP is a critical procedure, and so we’re sort of all stuck in a hard place right now, because you don’t want to completely remove our ability to do this, and yet obviously we need better scope design, because what we’re doing currently is just not working. And in our hands, doing this culture by the CDC guidelines wasn’t effective at identifying contaminated scopes.”
In addition to sending the scopes out for sterilization, Dr. Humphries’ team notified the 179 patients who had been exposed previously and offered them CRE surveillance. “At that time, just conveniently, all of the chromogenic media all of a sudden became unavailable for CRE surveillance,” she said, laughing. “So we adapted a technique that we use currently in the lab to look for carbapenem-resistant Acinetobacter. You inoculate your rectal swab onto the MacConkey plate and place meropenem disks, and then look for colonies that grow within a 28-millimeter zone. Anything that grows within that 28-millimeter zone, we do identification and susceptibility testing with the OXA-232 PCR.” They validated this method using some of their patients whom they knew were positive for OXA-232 and detected it in all of them. “We also did a seed-and-recovery study.”
The exposed patients were mailed swab collection kits with instructions. Of the 84 who had been exposed to one of the two high-risk scopes and who mailed back their kits, seven turned out to be colonized. None of the 95 patients who had been exposed to one of the other six scopes and who mailed back their kits proved to be colonized.
Dr. Humphries and her team had one question left. Since the index patient didn’t have a travel history, where did this come from?
“So we went back and screened all of our CRE from 2014 regardless of the imipenem MIC, and we did find one more patient who had OXA-232,” Dr. Humphries said. “This was a patient with travel outside the U.S. who came to UCLA for treatment. While he had several procedures done, he never did have ERCP. We are still investigating the possible epidemiological link with our index patient.” They did whole genome sequencing on his isolate, and he clustered in with their UCLA patient group. “So he probably is the source of this.”
“Why were we so lucky to go through all of this?” Dr. Humphries asked. Part of it could have been the environment, she said, noting Los Angeles does tend to have a high prevalence of CRE compared with other areas. And UCLA is a tertiary care facility, so a lot of patients with CRE are transferred in from other institutions. “And we had this very unusual organism that made us focus on this problem; otherwise we probably would have not even realized this was going on.” Then there is opportunity, she said: “We have an ongoing research in carbapenem resistance in our lab. We save all of our isolates, which is unusual, but again, is related to this research interest. And we have the ability to do pretty rapid development of tests and great collaboration with our hospital epidemiologists. Most importantly, we had these two really great post-docs who just took this project and ran with it and, really, I think, discovered the entire outbreak.”
[hr]
Anne Ford is a writer in Evanston, Ill.