Amy Carpenter Aquino
October 2018—How pregnancy affects normal thyroid function and thyroid function tests, and screening for thyroid disease during pregnancy, were the focus of a session at this year’s AACC annual meeting.
Ann M. Gronowski, PhD, DABCC, a professor of pathology and immunology, and of obstetrics and gynecology, Washington University School of Medicine in St. Louis, opened with an interactive question that addressed how the pregnant state affects normal thyroid function and thyroid function tests. Attendees disagreed on whether thyroid-stimulating hormone increases, decreases, or stays the same during pregnancy.
“You’re in the right place to find out,” Dr. Gronowski said. “The correct answer is that generally it decreases during the first trimester.”
Dr. Gronowski’s co-presenter was Joely A. Straseski, PhD, DABCC, of ARUP Laboratories.
Six main changes occur to the thyroid during pregnancy. The first one Dr. Gronowski addressed is that the high concentration of estrogen changes the thyroxine-binding globulin (TBG) glycosylation, which increases the half-life of the protein. The liver increases TBG production and reduces TBG clearance, which contributes to the two- to threefold increase in the amount of serum TBG concentrations. The TBG concentrations reach a plateau at about mid-gestation and remain elevated. “The affinity of T4 for TBG doesn’t change at all,” Dr. Gronowski said.
Second, as a result of the increase in TBG concentration, “you see a parallel increase in the concentrations of total T4 and total T3” around the 20th week of gestation. “Therefore, we can’t really use the normal reference intervals for total T3 and total T4.” The general practice is to multiply the upper reference level by 1.5 to get pregnancy-specific reference levels for total T3 and total T4.
Third, the protein hCG, which is a member of the pituitary glycoprotein family that has homology with TSH, LH, and FSH, can bind to the TSH receptor and has weak intrinsic thyrotropic activity. “During pregnancy, in the first trimester when hCG concentrations peak around weeks eight to 12, you see slightly decreased concentrations of TSH,” Dr. Gronowski said.
Surprisingly, only about three percent of women have an elevated free T4 concentration as a result. In this “kind of weird, inverse relationship,” she said, TSH decreases while hCG increases. TSH tends to stay within the normal reference interval, though some women may go outside the interval. A study she and colleagues conducted looked retrospectively at 16,000 physician-ordered hCG concentrations and found 69 samples from 63 women in which concentrations of hCG were greater than 200,000 IU/L (Lockwood CM, et al. Thyroid. 2009; 19[8]:863–868). “When you get concentrations above 400,000 IU/L, 100 percent of TSH in those women was below 0.2 mIU/mL. There is clearly this inverse relationship, especially as concentrations get very, very high.”

Dr. Gronowski
An increase in serum thyroglobulin is the fourth change to the thyroid during pregnancy. “Thyroglobulin itself lacks specific hormonal activity. Elevated concentrations can indicate increased thyroid status or injury to the gland. In pregnancy, it indicates an increase in activity.”
Thyroglobulin is produced by the follicular cells and is a precursor of the thyroid hormones. “Due to this increased demand for T4 in the first trimester, it’s associated with an increase in thyroid volume.” As pregnancy progresses, Dr. Gronowski said, “we shift to higher serum concentrations of thyroglobulin.”
An increase in renal iodine clearance is change No. 5. The increase in the glomerular filtration rate causes pregnant women to lose iodine renally, but this is compensated for by an increase in thyroid iodine clearance. This results in an increased dietary requirement for iodine, and in iodine-deficient areas it can result in goiter.
In the United States, where iodine intake is sufficient, the average increase in thyroid size is about 10 percent. In iodine-deficient areas, a size increase of more than 30 percent can be seen. Women in ancient Egypt and ancient Africa were believed to have tied a thin reed around their necks; when the reed broke as a result of goiter, it was an indication of pregnancy.
Change No. 6 is a decrease in serum free T4 concentrations. “You may see slight increases in the first trimester,” Dr. Gronowski said. “hCG concentration is high in its stimulant for thyroid.” The remainder of pregnancy, however, is marked by a decrease in serum free T4 concentrations. “This is due to the increase in TBG concentrations, the increase in renal iodine clearance, and an overall increase in the demand for T4.”
A 2007 study illustrated the decrease in free T4 whether measured by tandem mass spectrometry or immunoassay (Kahric-Janicic N, et al. Thyroid. 2007;17[4]:303–311). Despite the clarity of the measurements, “there’s been a lot of debate about this concept over the years,” she said. The question people ask is, “If TSH is normal, shouldn’t free T4 be normal?”
Dr. Gronowski referred to a 2009 study in which 93 nonpregnant patients were compared with 111 pregnant patients (Lee RH, et al. Am J Obstet Gynecol. 2009;200[3]:260.e1–e6). All patients were thyroid peroxidase antibody negative with no predisposition to thyroid disease and were screened using two immunoassay methods (Roche Elecsys and Tosoh A1A-600) to measure urinary iodine total T4 concentrations, TSH, and free T4.
The authors calculated the free T4 index, “a calculated value based on the total T4 concentration in the thyroid binding capacity,” one that provides a measure of the available thyroxin binding sites, Dr. Gronowski explained.
The index is not an estimate of free T4 concentrations, she said. “It’s just assessing if the amount of total T4 that’s there can be accounted for by the amount of binding protein that’s present,” similar to calculations for free versus total calcium.
The free T4 index “was valuable in an era when reliable, commercial free T4 assays were not available,” she added. “But now we have reliable free T4 assays, and we have free T4 by other, more reliable methods”—equilibrium dialysis and mass spectrometry.
The 2009 study examined nonpregnant and first, second, and third trimester TSH measurements, by immunoassay and mass spectrometry. “In the first trimester, TSH dropped slightly because hCG is rising, just as we expected,” she said.
The study’s authors looked at two immunoassay methods for free T4 and found a significant decrease in free T4 concentrations in the second and third trimesters with both methods.
In studying the free T4 index, however, researchers saw a slight increase in the first trimester only. “So they concluded that total T4 and the free T4 index retained an appropriate inverse relationship with TSH throughout pregnancy and appear to provide a more reliable free T4 estimate,” Dr. Gronowski said.
They were in favor of returning to the old method of the free T4 index because it maintains a relationship viewed as more appropriate. However, “they didn’t measure it by equilibrium dialysis, which is really what we consider the gold standard,” Dr. Gronowski said. “I would argue that there are conditions where you have this discordance between TSH and free T4,” she said, comparing it with euthyroid sick syndrome.
As illness progresses, “T3 decreases first, and eventually total T4 and free T4 will decrease as well. TSH generally stays within the normal range, and you’ll see an increase in reverse T3. That’s a natural process—the body is attempting to decrease the amount of T4 that’s converted to T3. I would argue that sick euthyroid syndrome is very similar to late pregnancy.”
In late pregnancy, free T4 and free T3 are low while TSH generally stays within normal limits. “Studies have shown that we see an increase in reverse T3, so it’s actually very similar to sick euthyroid syndrome, which makes physiological sense.”
 The difference between euthyroid sick syndrome and late pregnancy is that in pregnancy there is an increase in total T3 and total T4 because of the increased TBG. In euthyroid sick syndrome, “generally we see a decrease in total T4 and total T3. The difference is in the binding protein. We actually see this in other sick conditions, such as acute hepatitis B.”
The difference between euthyroid sick syndrome and late pregnancy is that in pregnancy there is an increase in total T3 and total T4 because of the increased TBG. In euthyroid sick syndrome, “generally we see a decrease in total T4 and total T3. The difference is in the binding protein. We actually see this in other sick conditions, such as acute hepatitis B.”
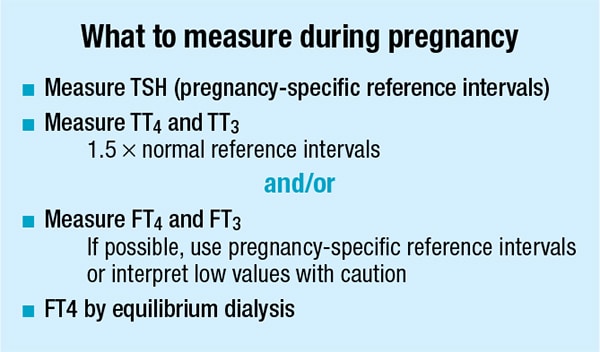
As for what to measure during pregnancy, Dr. Gronowski said, “We can reliably measure TSH. It’s handy if you have pregnancy-specific reference intervals. You can measure total T3 and total T4, adjusting the upper limit by 1.5. You can measure free T4 and free T3, and it’s useful to have pregnancy-specific reference intervals.” Many have been published.
“Our gold standard is always measuring free T4 by equilibrium dialysis. I don’t think we need to go back to free T4 index,” she added.
In an overview of normal fetal physiology, Dr. Gronowski said fetal thyroid follicles develop by 12 weeks of gestation, and by 13 weeks, fetal T4, TBG, and TSH concentrations have increased. T3 does not rise until the third trimester owing to late type I deiodinase production.
TSH and thyroglobulin do not cross the placental barrier. Estradiol and hCG are produced by the placenta, so they do cross over to the mother. Early in fetal development, maternal T3 and T4 cross the placenta, but the placenta becomes less permeable as the fetus begins to produce more T4. “It’s important to note, though, that hypothyroidism will still occur in the fetus even when the mother’s thyroid concentrations are normal,” Dr. Gronowski said. “Mom’s thyroid is not enough to compensate for a deficiency in an infant.”
Iodine, some drugs, thyrotropin-releasing hormone, and IgG immunoglobulin can cross the placental barrier.
Iodine deficiency during pregnancy is the No. 1 most prevalent cause of mental retardation. Recent data show that while the number of school-age children with iodine deficiency is declining in most parts of the world, the number of iodine-deficient children is increasing in the U.S., Dr. Gronowski said. She pointed to a few contributing factors: the popularity of iodine-free salts, iodized salts not being used in manufactured or commercially produced foods, and declining American salt intake in general due to concern about hypertension. “This is having an effect on iodine,” she said.
A 2010 study of pregnant, lactating, and nonpregnant-nonlactating women concluded that pregnant women were borderline iodine sufficient. Assessing iodine status should be performed by 24-hour or spot urine collection and measured by mass spectrometry, Dr. Gronowski said. Iodine should not be assessed on an individual basis, and routine screening is discouraged because of high day-to-day coefficient of variation in urine iodine.
Dr. Straseski, an associate professor of pathology at the University of Utah and ARUP’s medical director of endocrinology and co-director of the automated core laboratory, addressed the guideline recommendations for screening for thyroid disease during pregnancy. The American Thyroid Association in 2017 updated its 2011 guidelines for the diagnosis and management of thyroid disease during pregnancy and postpartum (Thyroid. 2017; 27[3]:315–389). In contrasting and comparing the two, Dr. Straseski zeroed in on the guidelines for TSH reference intervals, measurement of T4, thyroid autoantibody testing, and measurement of iodine, all during pregnancy.
TSH reference intervals were recommendation No. 1 in the 2011 guidelines, which said trimester-specific reference ranges should be used. The 2017 edition expanded on this recommendation by saying the population-based trimester-specific reference ranges for serum TSH should be defined by assessing local population data. Supporting data, from studies based in the U.S. and other countries, found many different reference intervals for TSH and free T4. “Reference intervals for thyroid function tests depend on the population studied and the trimester for some of these studies,” Dr. Straseski said. “They can also depend on the method. We need to be clear on what population these intervals are being used and we need to use them appropriately.”
The goal is to establish a range in a healthy population with no subclinical thyroid disease. The 2017 guidelines are clear about the inclusion criteria for TSH reference interval determination: In addition to being pregnant, women must be free from thyroid disease, have adequate iodine intake, and be thyroperoxidase antibody negative. “This would steer us toward a healthy population as it relates to thyroid disease,” Dr. Straseski said.
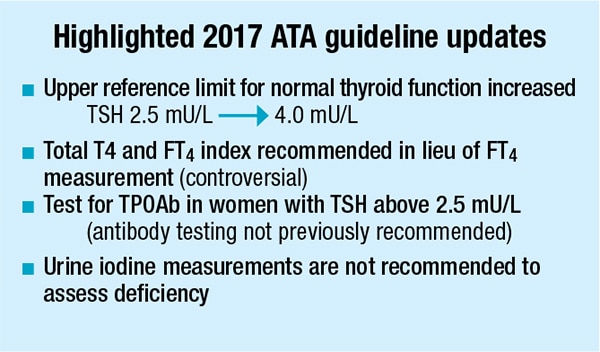
The TSH reference interval recommendations, which should be used only if internal ranges specific to the laboratory’s population are unavailable, are delineated by trimester. In 2011, the ATA recommended going up to a TSH value of 2.5 mIU/L for the first trimester and up to 3.0 mIU/L for the second and third trimesters. In the 2017 guidelines, an upper reference limit of 4.0 mU/L may be used in the first trimester. “That’s a full unit higher than it used to be,” Dr. Straseski said, calling it “a relatively big change.”
For the second and third trimesters, the ATA recommends referring to nonpregnant reference intervals, of which there are several. The ATA refers to one example of a nonpregnant reference interval with an upper limit of 4.2 mU/L, which is also a significant increase.
 The recommendations mention method-specific ranges but note that the variation seen between methods is not clinically significant. The guidelines also support the idea of using a multiple of medians approach to accommodate for differences between methods. The ATA specifically mentions that the 2017 recommendations for TSH reference interval ranges and consideration of method-specific and trimester-specific ranges also apply to the measurement of free T4.
The recommendations mention method-specific ranges but note that the variation seen between methods is not clinically significant. The guidelines also support the idea of using a multiple of medians approach to accommodate for differences between methods. The ATA specifically mentions that the 2017 recommendations for TSH reference interval ranges and consideration of method-specific and trimester-specific ranges also apply to the measurement of free T4.
“Everything I’m talking about for TSH goes for free T4,” Dr. Straseski said.
At last year’s AACC meeting, scientists from ARUP Laboratories were involved in two poster presentations that found a significant difference between pregnant and nonpregnant reference intervals and between trimesters. “This obviously is supporting the idea of population-based and trimester-based reference intervals,” Dr. Straseski said, noting that the upper limits determined using a particular immunoassay are similar to the limits reported in the ATA guidelines.
For the measurement of T4 during pregnancy, the Endocrine Society and the American Association of Clinical Endocrinologists support using the free T4 index.
In 2011, the ATA said that if free T4 measurement by LC-MS/MS was not available, any available method could be used to measure or estimate free T4. It also advised being aware of the limitations of each method and said TSH is more accurate than these alternative methods.
The 2017 guidelines say that measuring total T4 in lieu of free T4, with a pregnancy-adjusted reference range, is a highly reliable way to estimate hormone concentrations. Calculating the free T4 index to reach a free T4 estimation is acceptable also, the ATA said. But “free T4 index is considered by most of us in the laboratory community to be an outdated measurement,” Dr. Straseski said. “Free T4 index has been replaced by our contemporary immunoassays as well as direct measurement using LC-MS/MS. That was not always the case,” she said. “We know that free T4 index was in place in order to estimate the free T4, but we can measure that directly and, therefore, much more accurately now.”
LC-MS/MS using equilibrium dialysis or ultrafiltration as the sample preparation is considered to be the gold standard for measuring T4 and is recommended by the Endocrine Society and the ATA. “It performs well in this environment of high TBG, and that is obviously important in this population,” Dr. Straseski said.
ARUP Laboratories presented data at the 2016 AACC meeting that showed good correlation between each of four free T4 immunoassay methods and LC-MS/MS by ultrafiltration. “Better correlation than you might expect,” she said. A bias exists between immunoassay and mass spectrometry, of course, underscoring the need for method-specific reference intervals.
An abstract presented at the 2015 ATA annual meeting reported on adherence to the 2011 ATA guidelines and test use, particularly for new obstetric patients. Researchers in an academic institution reviewed 1,672 orders over six months to see if clinicians followed the then-guideline of reflexing to a free T4 in the presence of an abnormal TSH screen while using trimester-specific reference intervals. In one data set, which included patients with elevated TSH levels based on trimester-specific reference intervals, 94 percent had no free T4 follow-up. “It’s pretty clear they were not following those pregnancy-specific guidelines.”

Dr. Straseski
The second six-month data set in this study showed that half of all patients who had normal TSH levels in the context of pregnancy had unnecessary follow-up. “It’s important to think about the fact that you’re going to see a different interpretation, different follow-up, different clinical management, and diagnosis if you’re using nonpregnant reference intervals in the pregnant population,” Dr. Straseski said.
Another significant update to the 2017 ATA guidelines: “Pregnant women with TSH concentrations greater than 2.5 mU/L should be evaluated for TPO antibody status.” In 2011, the guidelines said there was insufficient evidence to recommend for or against screening all women for thyroid antibodies in the first trimester. The ATA calls for follow-up with a TPO antibody, Dr. Straseski noted, not the traditional reflex of a TSH elevation followed by a free T4. The European Thyroid Association recommends a free T4 as well as a TPO antibody test as follow-up to an elevated TSH. It goes one step further and recommends treatment for a woman who tests positive for TPO antibodies. If the TPO test is negative, the European Thyroid Association says that a thyroglobulin autoantibody test should be performed, Dr. Straseski said, “to make sure you’re covering your bases when it comes to those antibodies.”
The Endocrine Society and ACOG say there is no evidence on which to base a recommendation for universal screening for autoantibodies in these populations. “It will be interesting to see if there will be any changes” when they update their guidelines, she said.
For iodine status and nutrition, the ATA made no formal testing recommendations in 2011, though it did note that pregnant women required 250 mcg of iodine daily. The 2017 guideline says using median urine iodine concentrations can be used to assess the iodine status of populations but that single spot or 24-hour urine iodine concentrations are not a valid marker for the iodine nutritional status of individual patients. “We’re not routinely measuring iodine concentrations in these women, so in essence there has not been much of an update to this recommendation,” Dr. Straseski said.
With thyroid function critical to fetal development, and thyroid disease not uncommon during pregnancy, it may seem that most guidelines would recommend universal screening for thyroid function during pregnancy. This is not the case, Dr. Straseski said. “Actually, most do not say anything about this.”
She cited the pros of universal screening during pregnancy: missed diagnoses (representative studies show that only 30 to 80 percent of women with hypothyroidism would by identified by symptoms and risk factors alone), significant frequency (hypothyroidism is the second most common endocrine disorder affecting women of reproductive age), cost-effectiveness (most studies base costs on those associated with minimizing IQ loss), and benefit of treatment (unequivocal in overt hypothyroidism). Treatment benefit for subclinical disease is less clear, and that is one of the cons. Another con is cost-related: “Whether screening is cost-effective in this population depends on study statistics, on how they analyze their data.” However, “I think we can all agree that this is a critical diagnosis, and that alone makes some people say this justifies screening,” Dr. Straseski said.
Most major guidelines don’t recommend it. In 2011, the ATA said there was insufficient evidence to recommend for or against universal TSH screening at the first trimester visit. The 2017 update says the same. In 2011, the ATA said women at high risk for thyroid dysfunction may benefit from selected screening. “That statement is mimicked as well in 2017,” Dr. Straseski said. “Patients should undergo a clinical evaluation when we know they might be at risk.”
The Endocrine Society, AACE, ACOG, and the European Thyroid Association, all of which released recommendations between 2012 and 2015, do not advise universal screening of pregnant women for thyroid disease. However, each organization included a follow-up statement that supports testing for women at high risk for thyroid disease. “You just end up confused. I think it comes down to clinician preference as well as their experience if they know they have a case on their hands that they want to focus on,” Dr. Straseski said.
The risk factors that warrant screening for thyroid disease encompass such large groups of women, however, that “it ends up looking like universal screening anyway,” she said, citing just a few: history of diabetes, pregnancy loss, infertility, two or more prior pregnancies, and pregnancy after 30 years of age.
Dr. Straseski pointed to a significant update by the ATA regarding postpartum thyroiditis. The 2011 guidelines said women who have postpartum depression should have TSH, free T4, and TPO antibody tests. “The update in 2017 goes backward a little bit by making a much more general statement.” In 2017, the ATA said all patients with depression, including postpartum depression, should be screened for thyroid dysfunction. “This is due to the possible association between thyroid disease and postpartum depression,” but this is based on inconclusive studies, she said.
The Endocrine Society is the only other organization to address postpartum thyroiditis in its guidelines, and it says that women at high risk, defined as having type I diabetes, TPO antibodies, or a history of postpartum thyroiditis, should be screened via TSH. “They don’t mention the word ‘depression.’ I see quite a bit of difference between this and what the ATA is stating,” Dr. Straseski said.
Of the confusion created by the various organizations’ guidelines, Dr. Straseski said, “I look forward to giving this talk again in a few years with Dr. Gronowski as we continue to see what reveals itself in the literature.”
Amy Carpenter Aquino is CAP TODAY senior editor.