Amy Carpenter Aquino
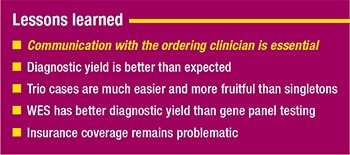
May 2019—Never go it alone without the input of the ordering clinician, and the diagnostic yield is better than expected. Those are two of the five lessons UCLA learned in its first seven years of clinical whole exome sequencing, said Wayne W. Grody, MD, PhD, in a session at last year’s Association for Molecular Pathology meeting.
UCLA Medical Center was an early adopter of next-generation sequencing. “Our group decided to focus first on heritable or germline variants for patients with undiagnosed or very rare diseases,” said Dr. Grody, director of UCLA’s molecular diagnostic laboratories and Clinical Genomics Center.
Stanley F. Nelson, MD, co-director of the Clinical Genomics Center, ran the high-throughput sequencing core for research purposes in the Department of Human Genetics. “We brought the clinical laboratory infrastructure to get CLIA certification for part of that laboratory, so we hit the ground running,” said Dr. Grody, who is also a professor in the medical genetics and molecular diagnostics divisions, Departments of Pathology and Laboratory Medicine, Pediatrics, and Human Genetics, UCLA School of Medicine.
Dr. Grody pointed to the published American College of Medical Genetics and Genomics/AMP standards and guidelines for interpreting sequence variants (Richards S, et al. Genet Med. 2015;17[5]:405–424) and warned against becoming overconfident in interpretation. A study published in 2016 of the performance of the ACMG-AMP variant-interpretation guidelines among nine expert laboratories revealed only a 34 percent concordance across laboratories (Amendola LM, et al. Am J Hum Genet. 2016;98[6]:1067–1076).
“That doesn’t bother me too much, because I really feel with clinical genome interpretation as practiced in medicine, a big portion of it is art as well as science,” Dr. Grody said. Even with ClinVar, for variants with two or more submitters, there is a classification discrepancy of about 17 percent. “This is of more than academic interest.”
Dr. Grody briefly reviewed the case of “the first, and to my knowledge only, lawsuit based on misclassification of a missense variant.” Christian Millare, of South Carolina, underwent next-generation sequencing as an infant. A missense variant was found on the SCN1A gene but reported as a variant of unknown significance (VUS), and the pediatric neurologist did not act on it.
“SCN1A is the gene for Dravet syndrome, a very severe congenital form of epilepsy that is known not to respond to typical anticonvulsant agents like Dilantin,” Dr. Grody said. It is treated with its own drugs, which have to be given in combination.
Christian went on to have seizures and did not respond to the anticonvulsant medications he received; he died at age three in status epilepticus. His mother sued (Amy Williams, et al v Quest/Athena) on the basis that if the variant had been called likely pathogenic, which is how it was subsequently reclassified, it would have been acted on and her son would have been prescribed the proper drugs and may have survived.
“Some of this reflects not only changing classifications, which are going to be with us forever, but misunderstanding by clinicians of what a VUS is,” Dr. Grody said. “It doesn’t mean it’s benign and it doesn’t mean it’s nonactionable. We only report VUSs that are in some form actionable.” The case raises important issues, he said, around the responsibilities of labs and clinicians to stay current and understand the appropriate translation of genomic sequence results to clinical care.
UCLA has a clinical genomics board that meets weekly to review cases and variants. After filtering out 25,000 of the variants that are likely benign, “we end up with a couple hundred to go through,” Dr. Grody said. The board consists of molecular/genomic laboratory directors and technical staff, genomic bioinformaticists, genetic counselors, clinical geneticists, pediatricians, residents and fellows, the specialists who have been seen, and the ordering clinicians, “who really know the patient’s phenotype better than we would.”
Dr. Grody
For internal UCLA cases, the clinicians are in the meetings and able to go through the variants in real time with the rest of the group. If the case is an outside referral, the ordering clinician is invited to join via web-based access.
“This is important because no one can know the whole genome, no one can know all those genes, all those diseases,” Dr. Grody said. “You could argue that it takes an expert center for every gene, every disease, but we can’t do that when we have 22,000 genes and a much smaller number of sequencing laboratories. We have to aggregate them somehow.”
One of UCLA’s first cases was a 17-year-old girl who had ataxia since age two and carried a longstanding diagnosis of juvenile ALS. When she arrived at UCLA Medical Center, however, the neurologists doubted the diagnosis of juvenile ALS. “They didn’t know what it was, so they ordered the exome sequence,” Dr. Grody said. “We found a homozygous, nonsense variant [E359X]—the parents were consanguineous—in a gene none of us had ever heard of before: AAAS, which is achalasia-addisonianism-alacrima syndrome,” also known as Triple A-S syndrome.“None of those three symptoms was in the medical note, at least not from UCLA,” except for the ataxia, which is also a feature of Triple A-S syndrome, Dr. Grody said. The pediatric neurologist was there, though, and confirmed that the patient had undergone years of motility studies for the esophageal symptoms of achalasia. She also found in the patient history a noted absence of tears (alacrima).
If the clinician had not been there to answer questions, “I may have not reported this at all, or buried it somewhere, because it didn’t really seem to fit the known phenotype,” Dr. Grody said. “It’s just a fact that if you’re in an academic medical center, unlike a commercial entity, the laboratory is one degree of separation at most from the treating physician. Sometimes it’s zero degrees because we have the person in the room.”
Dr. Grody shared a second exome sequencing case, one he said was recent and caused “a great deal of angst” owing to its ethical dilemma: A young girl presenting with a rare tumor that raised suspicion of a familial cancer syndrome. Exome sequencing revealed a known pathogenic variant in the P53 gene, diagnostic of Li-Fraumeni syndrome. But “there was also an incidental finding, if you can call it that”: The father’s DNA sample showed no relation to the child. “This compromises the informativeness of the exome report since it could not be determined whether the mutation was inherited or de novo,” meaning it did not come from the mother, he said. “And the real father could be at risk of cancer himself, without knowing it.” Yet there was resistance among the clinicians about including this finding in the report because of potential adverse effect on the family and because parentage testing had not been requested.
 Unexpected paternity results are nothing new in genetic medicine, but they are more frequent in “trio” exome sequencing, Dr. Grody said, which becomes a de facto paternity test and affects how the results are interpreted. The dilemma generated debate between the lab personnel and the clinical team, all of whom wanted what they felt was best for the family. “It’s the first case in about 20 years in which I actually consulted with our hospital ethics committee,” Dr. Grody said, noting that he usually is able to solve most ethical problems himself. “But this one was really difficult, and sure enough, the ethics committee also found it difficult.” The solution, a compromise of sorts, was to provide “some tactful genetic counseling” and was possible only because “all of us were on the same page—the genetic counselors, the oncologists, the laboratory directors, all of us involved with the patient.”
Unexpected paternity results are nothing new in genetic medicine, but they are more frequent in “trio” exome sequencing, Dr. Grody said, which becomes a de facto paternity test and affects how the results are interpreted. The dilemma generated debate between the lab personnel and the clinical team, all of whom wanted what they felt was best for the family. “It’s the first case in about 20 years in which I actually consulted with our hospital ethics committee,” Dr. Grody said, noting that he usually is able to solve most ethical problems himself. “But this one was really difficult, and sure enough, the ethics committee also found it difficult.” The solution, a compromise of sorts, was to provide “some tactful genetic counseling” and was possible only because “all of us were on the same page—the genetic counselors, the oncologists, the laboratory directors, all of us involved with the patient.”
The outcome of the case prompted UCLA to change its informed consent form to include a statement that unexpected family relationship results will be discussed and reviewed, and to perform a survey of other clinical genomics laboratories to compare approaches (Eno C, et al. Genet Med. 2019;21[4]:861–866).
The need for communication with the ordering clinician is first among the lessons learned from UCLA’s first seven years of clinical whole exome sequencing, Dr. Grody said. There have been many other cases at UCLA in which the presence of the clinical expert in the room “made all the difference in which variants were reported or not reported.” He cited some of the exome diagnoses that depended on clinical expertise: hereditary ataxias (e.g. SCA types 1–35), skeletal dysplasias (e.g. COL2A1), osteogenesis imperfecta type XIV (TMEM388) versus child abuse, immunodeficiency-14 (PIK3CD), hemophagocytic lymphohistiocytosis (PRF1), disorders of sexual development (e.g. SRD5A2), visceral myopathy (ACTG2), and autoinflammatory disorders (e.g. MEFV).Of the ataxia cases, Dr. Grody said: “I don’t know the clinical subtle differences between them—age of onset and what part of the body is ataxic. But we have neurology experts in the room who will be familiar with SCA type 23, for example, and say, ‘There’s no way that fits the phenotype.’ So we will not report it.”
“It doesn’t mean they are absolutely right all the time,” he added, “but as a result of this, our reports probably have fewer VUSs on them than many others, both commercial and academic laboratories.”
A recent case of multiple fractures and potential child abuse was an example of when not to recommend whole exome sequencing. “If you think it’s osteogenesis imperfecta, I would do the panel for that. If you open it up to all the genes, there’s going to be a VUS somewhere that a defense lawyer will grab ahold of and say, ‘See, it’s genetic,’” Dr. Grody said.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
