Julie A. Ribes, MD, PhD, director of clinical microbiology at UK HealthCare, Lexington, Ky., gave a presentation for surgical pathologists at CAP18 last fall on invasive parasitic infections. We reported in the January issue, in part one of our coverage, her cases of strongyloidiasis and paragonimiasis. This month: schistosomiasis, Naegleria fowleri, and maggots.
Karen Lusky
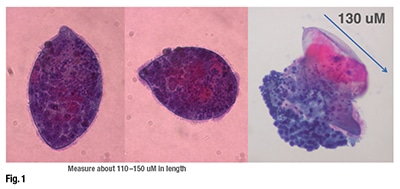 February 2019—In one case, Dr. Ribes found herself intrigued by structures in a patient’s urine cytology specimen. A 36-year-old man from the Republic of Congo had developed dysuria, increased urinary frequency, and terminal hematuria. What they found in the Pap stain in cytology, she said, were large purple structures with the knob at the end (Fig. 1). “If you look closely, you can appreciate the fact that these are ciliates. The predominant finding was these ciliated organisms present in the urine.” But there was more. In the same image on the right, Dr. Ribes pointed to a mass of cells, a little beak with cilia on it, and then “this sort of amorphous thing” on which she put a measure of 130 µm.
February 2019—In one case, Dr. Ribes found herself intrigued by structures in a patient’s urine cytology specimen. A 36-year-old man from the Republic of Congo had developed dysuria, increased urinary frequency, and terminal hematuria. What they found in the Pap stain in cytology, she said, were large purple structures with the knob at the end (Fig. 1). “If you look closely, you can appreciate the fact that these are ciliates. The predominant finding was these ciliated organisms present in the urine.” But there was more. In the same image on the right, Dr. Ribes pointed to a mass of cells, a little beak with cilia on it, and then “this sort of amorphous thing” on which she put a measure of 130 µm.
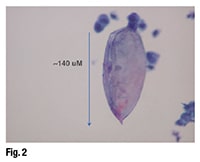 Everyone was focusing on the ciliates, but Dr. Ribes was concentrating on the other amorphous things. She displayed a structure that was 140 µm long, with a terminal spine at the end of it (Fig. 2). “There is no content to it,” she said, “because you can actually see that it has split open and whatever was inside has escaped.” This structure was the remnant of an egg shell.
Everyone was focusing on the ciliates, but Dr. Ribes was concentrating on the other amorphous things. She displayed a structure that was 140 µm long, with a terminal spine at the end of it (Fig. 2). “There is no content to it,” she said, “because you can actually see that it has split open and whatever was inside has escaped.” This structure was the remnant of an egg shell.
What has escaped? she asked. When Dr. Ribes thinks about Schistosoma haematobium infection, she is reminded, she said, “of the wet mount in microbiology, which has the very classic egg that has the very nice terminal spine.” Inside the egg one expects to find a miracidium, a ciliated stage of development for the schistosomes. On further investigation, Dr. Ribes found one structure that still had the miracidium inside and somewhat of a terminal spine. And it was within what the Centers for Disease Control and Prevention says is the size range (112–170 µm in length) for S. haematobium eggs. Dr. Ribes observed more eggs with “the miracidium, the ciliate, emerging from them, oftentimes with inflammatory cells derived from the patient.”
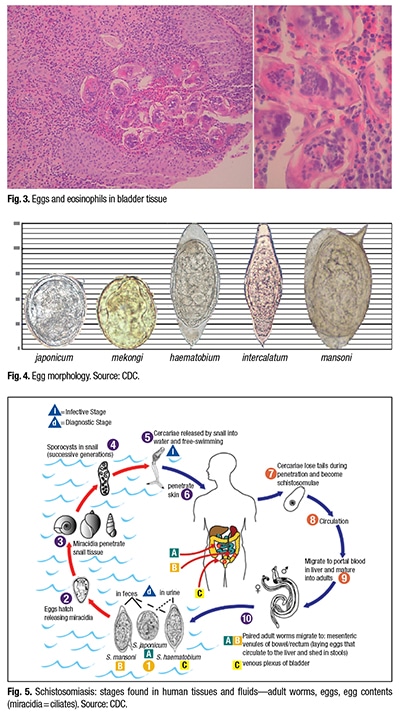 The patient also had a mass in his bladder wall. “So they biopsied that,” Dr. Ribes said, describing the specimen as having structures with “wavy and contorted edges that you would like to say look like eggs, and actually they are eggs and they do have contents in them.” She pointed out miracidia inside the eggs (Fig. 3), noting that the egg in the middle looked perhaps like it had a terminal spine. “But this is all wavy and all crunched up. It’s hard to know which is your long axis, or if this is the entire long axis.” The take-home message, she said, is that determining size and morphology of eggs in tissue sections may be challenging. Correlating with the morphology seen in cytology or ova and parasite wet mounts of stool is important for definitive identification.
The patient also had a mass in his bladder wall. “So they biopsied that,” Dr. Ribes said, describing the specimen as having structures with “wavy and contorted edges that you would like to say look like eggs, and actually they are eggs and they do have contents in them.” She pointed out miracidia inside the eggs (Fig. 3), noting that the egg in the middle looked perhaps like it had a terminal spine. “But this is all wavy and all crunched up. It’s hard to know which is your long axis, or if this is the entire long axis.” The take-home message, she said, is that determining size and morphology of eggs in tissue sections may be challenging. Correlating with the morphology seen in cytology or ova and parasite wet mounts of stool is important for definitive identification.
Schistosome eggs are large, with the largest ones—S. mansoni, S. haematobium, and S. intercalatum—more than 100 µm long. Schistosoma japonicum and S. mekongi eggs are rounder and smaller (Fig. 4).
“We don’t have human schistosomes in any waters in the United States,” Dr. Ribes says. “Schistosomiasis is re-emerging in parts of Europe.” An online CDC document lists some of the countries and areas of the world in which each of the five species can be located, among them Africa, the Middle East, Indonesia, Cambodia, and Laos (www.cdc.gov/parasites/schistosomiasis/epi.html).
Schistosomes have complicated life cycles with one intermediate host (Fig. 5). In the case she shared, the eggs were shed from the human in urine; in many other instances they’re shed from stool. “These eggs will hatch once they are out in the environment and are ready to search for that next stage in their life cycle, which is the snail. The miracidia will infest the snails, in which there will be a huge amplification of the organism. The cercariae are then released from the snails and are ready to invade the next host.”
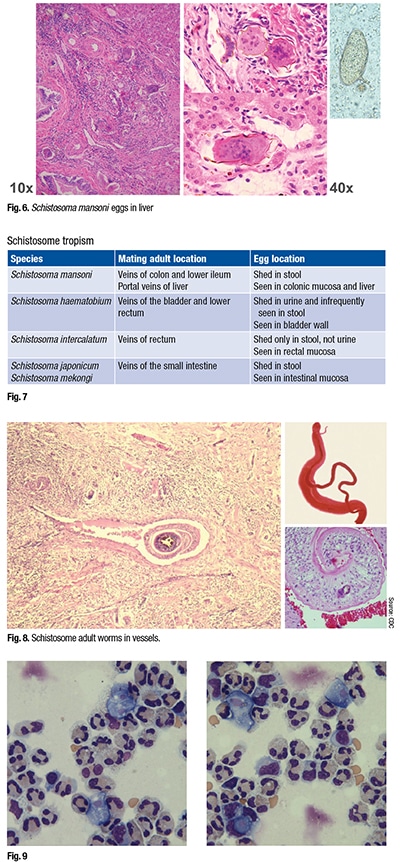 In this case, the human host is wading or swimming in snail-infested waters, Dr. Ribes said. “The cercariae will directly penetrate the skin” and then gain access to the venous system. “They will then go and hang out until mature in the portal venous system.”
In this case, the human host is wading or swimming in snail-infested waters, Dr. Ribes said. “The cercariae will directly penetrate the skin” and then gain access to the venous system. “They will then go and hang out until mature in the portal venous system.”
Schistosomes, which have two different sexes, mate up for life and migrate together to their target vessels. S. haematobium will go to the venous system that supplies the bladder. “For other schistosomes, it will be the colon, or the small bowel, or the portal system (Fig. 6). They will hang out in those vessels, and then do what they do for a living, which is produce more eggs.” (Fig. 7).
Dr. Ribes displayed an image of a biopsy from another patient showing schistosomes in a vessel (Fig. 8, left image). “You can see there are two of them; the female is the round structure that is in the middle, and the male holds her in what is referred to as a copulatory groove,” she said. On the top right, “You can see that the wider of the two is the male, and there is the female that is held in copula.” Dr. Ribes said the tissue tropisms, as she had mentioned, occur after the organisms are adults. Then “the female and male exit together in copula and head toward the target veins they are most happy living in.”
In the same tissue (the image on the lower right from the CDC), Dr. Ribes noted a single male schistosome that seems to have been “unlucky in love.” So he went searching for a mate and wound up in the lung, which is unusual for schistosomes to do. “But if you are still looking for love, you can look for it in the wrong places. So it’s sort of a recurrent theme with some of these flukes that you may find them in tissues that perhaps you weren’t expecting to find them in.”
Tissue tropisms may suggest a particular schistosome, she said, but schistosomes don’t always “read the book, so correlate with egg structure.” (Fig. 4). “Always thinking like a microbiologist, you measure up. You think about the life cycle [and] the tissue tropisms to help you make the diagnosis,” she said. “And then you do the clinical correlate with the type of specimen you are happy to measure the eggs in,” which, for schistosomes, usually is going to be stool or urine.
Every year in the United States, a few patients die from the brain-eating ameba Naegleria fowleri, says Bobbi Pritt, MD, MSc, DTM&H, director of the clinical parasitology laboratory at Mayo Clinic in Minnesota. “It’s usually devastating,” because a young child became infected by swimming in a freshwater lake or, rarely, an inadequately chlorinated swimming pool. The water containing the amebae goes into the roof of the nose, which communicates with the brain, Dr. Pritt said in an interview, noting that Minnesota has had two such cases within the past 10 years.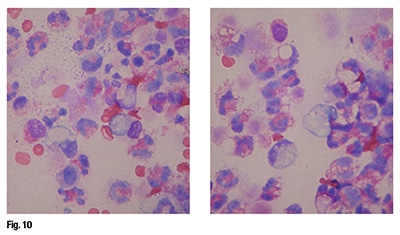 Laura Stadler, MD, MS, a pediatric infectious disease specialist at UK HealthCare, recalls several years ago a female pediatric patient with N. fowleri primary amebic meningoencephalitis. The child died, and in an effort to have “something good come of the situation,” Dr. Stadler says, and to raise awareness and educate clinicians, she and Dr. Ribes and another UK HealthCare colleague published the case as a photo quiz, “Ten-year-old with fever, headache, and neck stiffness” (Myint T, et al. Clin Infect Dis. 2012;55[12]:1677, 1737–1738).
Laura Stadler, MD, MS, a pediatric infectious disease specialist at UK HealthCare, recalls several years ago a female pediatric patient with N. fowleri primary amebic meningoencephalitis. The child died, and in an effort to have “something good come of the situation,” Dr. Stadler says, and to raise awareness and educate clinicians, she and Dr. Ribes and another UK HealthCare colleague published the case as a photo quiz, “Ten-year-old with fever, headache, and neck stiffness” (Myint T, et al. Clin Infect Dis. 2012;55[12]:1677, 1737–1738).
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
