CMS finalizes HbA1c coverage
Charles Fiegl
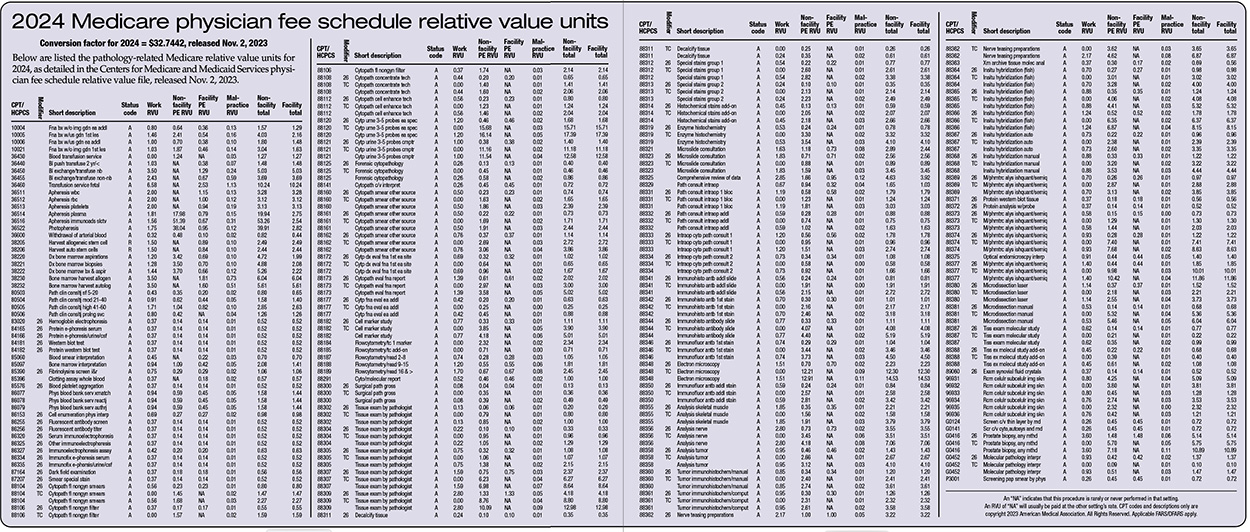
December 2023—In the 2024 Medicare physician fee schedule final rule, the Centers for Medicare and Medicaid Services reacted favorably to the CAP’s advocacy to mitigate payment decreases to pathologists next year. Overall, payments to pathologists are expected to decrease by an estimated 2.7 percent.
Pathologists were projected, at the beginning of 2023, to receive a Medicare cut of 6.5 percent starting in 2024. Other physician specialties were facing similar cuts because this reduction was driven largely by G2211, a new evaluation and management add-on service developed by the CMS and expected to be implemented in 2024. Due to budget neutrality requirements in the Medicare physician fee schedule, the add-on service had to be offset by cuts to other physician services elsewhere in the fee schedule. At the same time, physicians who relied mainly on office or outpatient evaluation and management visits, such as primary care specialties, were assumed to have relatively high use of G2211 and would experience overall increases to their payments next year.
The CMS has said code G2211 reflects the time, intensity, and practice expenses required to build longitudinal relationships with patients and address most of their health care needs with consistency and continuity over long periods. However, the CAP has contended that the implementation of G2211 essentially allows duplicative billing because the work captured in code G2211 is already described and accounted for within the existing evaluation and management CPT code set. The CAP and other physician specialties negatively affected by the add-on code’s introduction successfully lobbied Congress to delay payment for G2211 in 2021 for three years given the impact it would have during the pandemic.
When the CMS published the proposed 2024 fee schedule in July 2023, the Medicare program, after more lobbying by the CAP and other specialty physician organizations, made adjustments to how often G2211 would be billed. The CMS revised its assumptions that the code will be used during 90 percent of all evaluation and management patient visits to it being billed 38 percent of the time initially in 2024 and 54 percent of the time when fully adopted in future years. The lower use of the service reduced the budgetary impact to the whole fee schedule, including pathology and laboratory services.
The CAP is still opposing implementation of the add-on code and has joined specialty physicians to ask Congress to again take action. Congress is unlikely to do so, however, because of support for the service from primary care physician specialties and other groups.
Other actions by the CAP have had a positive impact on the Medicare physician fee schedule for pathologists and independent laboratories.
For example, this year the CAP directly advocated to the CMS for a 12 percent increase to the cytotechnologist clinical labor rate used by the federal agency in its practice expense methodology to calculate pathology payment. This increase was supported by public wage survey data and more accurately reflects cytotechnologist education, job duties, workforce shortages, and recruitment challenges. The CMS agreed with the CAP request and finalized a two-year, phased-in increase starting in 2024.
The CAP last year advocated for a separate increase to the histotechnologist clinical labor rate. The increase was finalized in the 2023 Medicare fee schedule and continues to be a benefit to pathology services as it is implemented over three years. As a result of these two policies, many pathology services will experience an increase to their technical component and global payments in 2024 and 2025.
In addition to the CAP’s efforts to improve the labor inputs, the CMS acknowledged the AMA-led physician practice information survey for 2023–2024, the primary purpose of which is to collect representative data on practice expense and hours spent in direct patient care. The CAP throughout much of 2023 promoted pathologist participation in the survey. The data will be collected at the specialty level and shared with the CMS to update the Medicare Economic Index and practice expense relative values on the physician fee schedule. The AMA has contracted with Mathematica, an independent research company with extensive experience in survey methods and in care delivery and finance reform, to conduct the survey.
Concerned that the survey does not fully capture the breadth of pathology practice because it excludes independent laboratory practices, the CAP contracted with Mathematica to run a supplemental survey to capture the same level of data but for laboratories billing Medicare services with Medicare specialty code 69 (clinical laboratory). This separate survey effort will launch in January and be open through April 2024. Mathematica will clean, process, and analyze data in summer 2024; summary statistics and result reports will be ready by late fall 2024. Independent laboratories should be on the lookout for two surveys from Mathematica. The first will seek practice expense information from individual practices, and the second survey will collect patient care hour data from individual physicians.
The CMS proposed in July adding the HbA1c test to the types of diabetes screening tests covered under Medicare, consistent with a recently revised recommendation of the U.S. Preventive Services Task Force, and has finalized its proposal to do so.
The CMS proposed expanding coverage of diabetes screening tests to include hemoglobin A1C, expanding and simplifying the frequency limitations for diabetes screening, and simplifying the regulatory definition of “diabetes” for diabetes screening, medical nutrition therapy, and diabetes outpatient self-management training services.
The CAP’s proposed rule comment letter to the agency said the HbA1c test is clinically appropriate for diabetes screening and has unique advantages, compared with existing covered tests, that the practitioner and patient should consider when choosing a diabetes screening test. The CAP supported the expansion of coverage to include the HbA1c test for diabetes screening, as well as the expansion and simplification of the frequency limitations.
The finalized 2024 conversion factor used for the fee schedule’s payment formula is $32.7442 and represents a 3.37 percent decrease from the 2023 conversation factor.
The decrease would have been lower if not for a 1.25 percent increase included in the Consolidated Appropriations Act of 2023. The CAP lobbied Congress throughout 2023 to mitigate cuts to pathologists further. In early November, the Senate Finance Committee drafted and voted out of committee legislation that would mitigate the 2024 cut by an additional 1.25 percent. At this article’s deadline, Congress had not yet acted on the bill as negotiations to appropriate funds for fiscal year 2024 federal spending continued.
Charles Fiegl is director of CAP advocacy communications, Washington, DC.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management