
Dr. Feldman
“I like the approach they have taken, building a separate Web services application —no vendor handles this well yet—that talks to the pathology and radiology back-end and integrates into the EMR as a report. It gets at some low-hanging fruit on integrated reports,” Dr. Feldman said via email. “The value of integrated reports is to avoid errors of omission—not commenting on a lesion that is radiographically evident but not represented on the pathology biopsy; errors of commission—wrong size is documented; or documenting multiple lesions for molecular studies to understand heterogeneity.”
Dr. Feldman, associate professor of pathology and laboratory medicine at the University of Pennsylvania’s Perelman School of Medicine, says he and his colleagues are working on an integrated diagnostics project but that it is too early to share details.
“We are trying to develop something new and novel,” he said. “Fingers crossed, we can pull it off. We are just getting going on this. Hopefully, we will have something to write about in 12 months’ time.”

Dr. Friedberg
Dr. Friedman, of the University of Michigan Medical School, sees the UCLA system as a step forward.
“That’s outstanding, and it’s a kind of a blending of information technology,” he says. “When you’re talking about an integrated view on the diagnostic side, you’re talking about pathologists, radiologists, sometimes cardiologists who act as their own diagnosticians, coming up with a unified note on diagnosis. That doesn’t have to be people sitting around in a room. At UCLA, they are doing it with technology. Some cases may be so complex that people do a teleconference.”
Baystate’s Dr. Friedberg sees the UCLA effort as a high-tech adaptation of a standard method of multidisciplinary collaboration.
“Every academic medical center has some flavor of tumor board or academic conferences where radiologists are representing their component and pathologists are presenting their component,” Dr. Friedberg says. “When you look at places like UCLA and what I’ve heard about it, it’s a natural evolution of that.”
At Baystate, clinical diagnostic functions remain fairly separate, but the past few years have seen a greater sharing of administrative functions.
“I had no desire to merge radiology and pathology, because we can merge the administrative side in our environment. In sales and marketing, for example, we have a good-sized reference lab as part of the department with a significant outreach component. If I’m looking to bring on, say, a nursing home as an outreach client for the hospital, the fact that we have access to a mobile x-ray machine if they need it, because of our connection to radiology, is a tremendous advantage,” Dr. Friedberg says.
“It’s an easier and more logical construct for them to understand. ‘You guys take care of the diagnostics. If we have a diagnostic question, whether it’s in urinalysis or an x-ray or talking to pathology or radiology about a case, I want to think of one diagnostics operation.’ So, I can see us in a world where there’s the diagnostic component and the therapeutic component, and we are the diagnostic component.”
The extent to which the idea of integrated diagnostics can be implemented depends greatly on local factors, he adds.
“You will find some places that take more advantage of it because they’re in a microenvironment in terms of politics, payers, and power structure inside the health system that it’s going to go farther than others in terms of being more formalized.”
Part of that “microenvironment” is the technological hurdles that must be overcome to enable frictionless, real-time pathology-radiology collaboration, Dr. Friedberg says.
“Any organization that can facilitate the interface in a way that works and improves the information flow that is so crucial to diagnostics, to provide the right information with the right context at the right time, that’s going to be a tremendous advantage,” he says. “But that will require somebody to have the pathologists and the radiologists and the labs and molecular guys and the geneticists all talking to each other.”
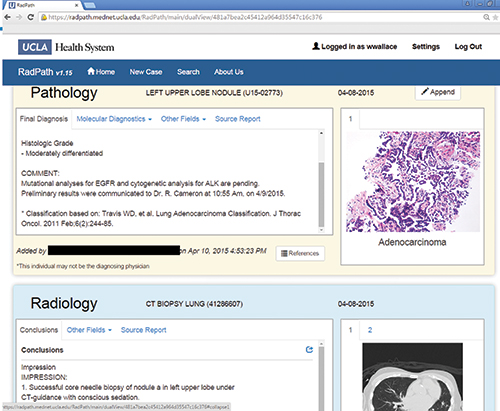
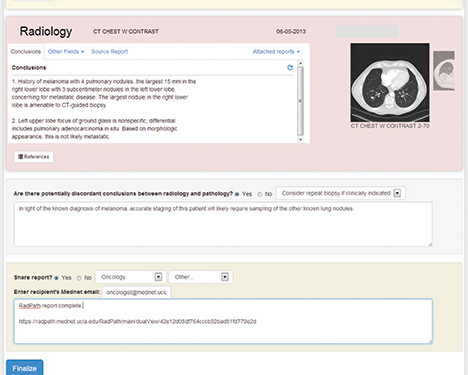
Screenshots offer a sample of how UCLA’s RadPath system gives clinicians a single diagnostic report (left) and offers pathologists and radiologists a means to find and resolve discordances (right). Source: May 5, 2014 Executive War College presentation by
Drs. Wallace and Arnold.
Back at UCLA, the team that developed its homebrew integrated diagnostic reporting system addressed the technological complications by using the Java Platform, Enterprise Edition, computing platform. UCLA pathologists are charged with initiating the integrated reports after they sign out the case in the LIS. Then the partner in radiology is alerted that the case is ready for review now that the pathology findings are in. As for determining who in radiology would do the correlation, workflow was an important consideration.
“It doesn’t take a whole lot of time, but time is money,” Dr. Arnold said at the War College. “Our initial thought was that the original diagnostic radiologist should perform this correlation. Now they would know the true diagnosis and could say which one of their differentials it wasn’t.”
The problem with that approach, Dr. Arnold said, was twofold. By the time the biopsy has been done and the pathology report completed, it may have been weeks since the diagnosing radiologist examined the radiological images and so she would have to look at all the images again to refresh her memory. Meanwhile, the diagnosing radiologist would not necessarily know the biopsy’s outcome or even whether it was done at UCLA.
“So we considered the biopsy radiologist,” Dr. Arnold said. “They didn’t necessarily perform the diagnostic interpretation, but they would have reviewed the previous one if it existed.” And these radiologists would, of course, know the biopsy outcome and have the most recent familiarity with the cases.
“In our framework right now, the biopsy radiologist is the one who performs the correlation. Also, this is due to the fact that we have a lot of interventional radiologists who are very enthusiastic about doing this,” Dr. Arnold added.
If a discordance is spotted, the radiologist can choose a reason from a drop-down menu. These choices include “Defer to pathology diagnosis,” “Combined findings suggest sampling error,” “Consider repeat biopsy if clinically indicated,” or “Other,” with a text entry box for comment. An example comment shown during the presentation for a biopsy showing lung cancer was, “In light of the known diagnosis of melanoma, accurate staging of this patient will likely require sampling of the other known lung nodules.”
Once completed, a link to the RadPath report can be emailed to the ordering clinician.
Given the extra steps the RadPath reporting system requires pathologists and radiologists to take, that big question of time was one Dr. Wallace and his UCLA colleagues were keen to measure carefully when rolling out the project late last year. What did they discover? Usually, the diagnostic concordance process takes seconds to complete, with nearly two-thirds of cases completed in a minute or less. Because radiologists do the correlation, it typically takes them longer to complete their portion of the job.
Dr. Wallace says there are plans to expand the RadPath system beyond lung cancer.
“We’re currently working on bringing up a prostate RadPath correlation report. . . . The liver service line also wants to start using this system. Then after that, probably breast would be a natural choice for this expansion.”
Could the RadPath system be exported to other health systems interested in giving it a go? Dr. Arnold, the informaticist who played a key role in overcoming the technical hurdles to diagnostic integration, had this to say.
“It’s fair to mention that this idea started [at UCLA] in 2008, and there was a system in place that was rather time-consuming. I came in 2012 and brought a Web application perspective to it that helped expedite things. One of the things that’s an ongoing challenge is the variety of ancillary systems. We developed the application with distinct layers of logic so it could go to Stanford or the University of Pennsylvania, and they would only need to modify the interface code to plug in and work with their systems,” he says. “The other side is that while we do have those aspirations, we are not really a software development company. We have looked at partnering with other places, and those conversations are ongoing. But our No. 1 priority is to make sure that the system being developed here meets our clinical needs.”
Penn’s Dr. Feldman, for one, voiced a strong interest in an off-the-shelf option that he and his colleagues could use to facilitate electronic pathology-radiology consultation.
“It would be really nice if the commercial vendors got into this space,” he said.
Officials at Xifin, the software-as-a-service vendor widely known for its laboratory billing solutions, hope they have the answer to Dr. Feldman’s wish. This spring, the company announced a partnership with teleradiology firm Virtual Radiologic—vRad for short—to develop a cloud-based solution aimed at facilitating consolidated diagnostic reports of radiology, pathology, and laboratory results.
vRad’s 350-plus physicians interpret more than 5 million patient studies every year. Xifin, meanwhile, recently purchased VisualShare for its image-sharing technology.
“vRad is very experienced in moving images. They are the largest radiology group in the world, and they move over 1 billion images annually. So they understand the workflow when it comes to moving radiology images,” says David Byrd, Xifin’s vice president of business development. “We really understand the laboratory and pathology side of the business, plus we have the platform to support both pathology and radiology images and a host of other images with the content. There are strong synergies between the two companies that really formed the partnership.”
Their product, now available, is called Xifin ProNet MDT. Those last three letters, MDT, are meant to highlight the solution’s aim of enabling multidisciplinary team collaboration as well as integrated diagnostic reporting.
“What’s important about this solution is that it allows multiple specialties, including radiology, pathology, and oncology, to communicate together as a team,” Byrd adds. “Cancer cases can take anywhere from a year or two, if not longer. And what the system is doing is not only creating a consolidated diagnostic report to share with the clinician, but allowing real-time and asynchronous communication to go on within the team.”
Byrd argues that facilitating that discussion could not only improve histology-imaging concordance but also help provide high-quality cancer care more efficiently by cutting needless testing.
“It’s not just about pathology and radiology communication,” he says. “It’s creating a value-based care plan that’s obviously impacting the outcome of the patient in a more positive way, while also saving the health care system dollars.”
When a case is flagged as being of interest, which can be done by the pathologist or the radiologist working within their RIS or LIS, the related images and findings are uploaded to the Xifin platform, says Bill Taylor, the company’s chief marketing officer. Other members of the care team are alerted that there’s a case available to review. Taylor says Xifin’s product should be attractive to a wide range of health care systems interested in pursuing integrated diagnostics.
“What UCLA has is a proprietary system just for UCLA,” he says. “What we’re building is a commercial offering. Our platform is completely agnostic to the instruments, the scanners, viewers, PACS, LIS, RIS, EMR, or EHR.”
Xifin ProNet MDT is in use at an undisclosed proof-of-concept site, but has no other users yet. Xifin account manager Sandra Martins is meeting with potential clients.
“We have a lot of people who are very interested in this solution and in this collaboration,” Martins says. “Some of the accounts we’re speaking with have explained that in their workflow today, all pathologists, radiologists, and oncologists are working in silos, and that they like the ability to connect that we give them. Within minutes, they have access to all of the images, the whole-slide imaging, the DICOM images, and all the text and the metadata that comes with it, to review from anywhere. It’s a cloud-based solution, and that capability is one of the strongest points.”
She says, however, that not everyone sees the potential benefit given how health care is changing.
“There are some organizations out there that don’t have the vision or the understanding of where we’re going, and that’s one of the biggest challenges,” she says.
Hostility to that “vision thing” (as the first President Bush put it) also is proving to be a challenge for Gabriel P. Krestin, MD, PhD, pathology chair at Erasmus MC University Medical Center Rotterdam in the Netherlands. He and his colleagues are attempting to implement some elements of the integrated diagnostics plan outlined by Dr. Friedman but are running into headwinds. They are developing complex, integrated diagnostic algorithmic order sets with the aim of cutting short the diagnostic odyssey.
“This is the ultimate goal,” Dr. Krestin says. “This is something you will do in some selected, difficult cases because it’s very resource-intensive.”
The notion of algorithm-driven ordering of appropriate diagnostics has encountered fierce resistance from clinicians, who see stronger direction from the diagnostic specialties on how to proceed with testing as a usurpation of their role.
“We ask and you do. This is the concept they have,” Dr. Krestin says. There are also uphill battles to climb among pathologists and radiologists who are hesitant to collaborate to develop integrated order sets.
“The laboratory medicine specialists know nothing about imaging. The imaging specialists know nothing about laboratory medicine, and don’t care about it. They say, ‘We have enough work to do. Why should we take this on?’”
Dr. Krestin speculates that growing specialization—experts who subspecialize in brain imaging and brain pathology, for example—may offer the best chance for multidisciplinary collaboration that improves diagnostic accuracy and efficiency.
“We have to find ways of breaking the silos and barriers between the specialties,” he says.
One way to improve pathology-radiology collaboration may be to knock down those walls before they are built. That is part of what is driving a new initiative for pathology and radiology trainees at the University of Kansas Medical Center, or KUMC.
For years, pathologists and radiologists there have led the way in multidisciplinary collaboration (see “AP, radiology talk it out on breast cancer cases,” CAP TODAY, August 2012, page 50). They hold weekly, hourlong, breast radiology-pathology Web video conferences in which all benign lesions are reviewed for potential discordances.

Dr. Tawfik
“The question is how negative is a negative?” says Ossama Tawfik, MD, PhD, director of anatomic and surgical pathology at KUMC. “We in pathology say a positive means it’s positive, but a negative does not really mean it’s negative.”
That work, started in 2008, revealed that the initial diagnostic reports agreed only 65 percent of the time. Of the rest, 34 percent required rebiopsy, x-ray of tissue blocks, or some other step before concordance on the finding could be reached. In 0.3 percent of patient cases, the patient was diagnosed, upon review, with ductal carcinoma in situ. Extrapolating from the KUMC findings, a November 2010 Department of Health and Human Services Report, “The Importance of Radiology and Pathology Communication in the Diagnosis and Staging of Cancer: Mammography as a Case Study,” estimated that, nationwide, nearly 10,000 breast cancer diagnoses are missed annually because of undiscovered diagnostic discordances.
Mark L. Redick, MD, PhD, helped bring the weekly breast conferences into being and sees the idea slowly gaining acceptance elsewhere.
 “At national meetings, this used to be an occasional topic you’d hear discussed maybe every two or three years,” says Dr. Redick, assistant professor in the radiology breast imaging section at the University of Kansas Cancer Center. “Now there are regular, dedicated portions of all the major breast meetings talking about this process. There’s improved appreciation for the need and more places are doing it. . . . Now with some competitors in our marketplace, we are seeing radiology-pathology addendum reports that never used to be provided.”
“At national meetings, this used to be an occasional topic you’d hear discussed maybe every two or three years,” says Dr. Redick, assistant professor in the radiology breast imaging section at the University of Kansas Cancer Center. “Now there are regular, dedicated portions of all the major breast meetings talking about this process. There’s improved appreciation for the need and more places are doing it. . . . Now with some competitors in our marketplace, we are seeing radiology-pathology addendum reports that never used to be provided.”
He adds that liver, lung, and other areas at KUMC are weighing whether to incorporate collaborative conferences of the kind being done with breast cases. One barrier, he says, is that these areas lack the volume of cases to make weekly conferences worthwhile and that stretching out the meetings would unduly delay final diagnostic reports to physicians and patients.
Dr. Tawfik, who directs the KUMC surgical pathology fellowship program, decided along with his colleagues that “it was time to expand the experience” of pathology-radiology collaboration by involving trainees.
“We created a curriculum for our residents where they get together and we talk about classic features or challenging situations for radiologists and pathologists in an integrated way,” he says. “There’s a radiology expert and a pathology expert and each presents three to five cases highlighting the issues, with teaching points or challenging points about what to do for each situation.”
The quarterly program, started in September 2014, has been “very well received.” Trainees in pathology and radiology are required to attend.
So far, lectures have focused on breast, musculoskeletal, thoracic, and hepatobiliary cases drawn from KUMC patient files, says Shelby Fishback, MD, the radiology residency program director.
“We’re not just covering bread-and-butter cases like appendicitis, but looking at some higher-level diagnoses. That takes expertise on the imaging and pathology side of things, so it’s a cool meeting of the minds,” Dr. Fishback says.
The radiology residents appreciate seeing the pathology-proven diagnoses in cases. “That makes us better imagers,” she says, “because it gets the actual diagnosis for troubling cases and refines our interpretation of cases going forward.”
Katie Dennis, MD, who directs the pathology residency program, sees a similar benefit for her trainees.
“The pathology residents are learning a lot from this conference, especially why it is important for them to correlate what they are finding in the gross specimens back to what the radiologists found,” she says. “And they like the direct interaction with the radiology residents.”
Dr. Fishback agrees, noting the quarterly lectures help on a basic level of putting a face to a name.
“I’ve met some of the pathologists who I’d only seen their name on reports. This definitely increases collaboration because of that familiarity between the departments. The radiology residents now feel like they know some of the pathology department people.”
Such familiarity could lead to collaboration on case write-ups or research projects, Dr. Fishback says.
The CAP’s Dr. Friedberg cautions that whatever may come in the realm of pathology-radiology collaboration or integration, such initiatives should not be mistaken for a merging of the specialties.
“People need to realize we’re not talking about turning pathologists into radiologists, or radiologists into pathologists. We’re talking about taking expertise and analyzing information,” he says. “We have to think of ourselves as tool independent. We have to think of our role in the health care system as one in which we are applying science to the care of our patient. It’s going to be a fun ride.”
[hr]
Kevin B. O’Reilly is CAP TODAY senior editor.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
