Amy Carpenter Aquino
September 2023—A casual comment made in a routine exchange in an Avera McKennan Hospital laboratory sparked a five-year campaign to bring down the urine culture contamination rate.
“I feel like all I do is report contaminated cultures,” a microbiology technologist said in 2016. “That started the ball rolling,” says Kacy Peterson, MBA, MLS(ASCP)CM, DLM(ASCP), laboratory service line administrator at Avera McKennan Hospital and University Health Center, Sioux Falls, SD. It wasn’t a monitored quality indicator at the time, so Peterson and her colleagues dug into the data. “We were shocked to find that our microbiology technologist was right. Forty-five percent of the time those cultures she was reporting were contaminated.”
At the Association for Diagnostics and Laboratory Medicine (formerly AACC) meeting in July and in an interview shortly after, Peterson shared her laboratory team’s journey to a lower contamination rate and fewer unnecessary urine cultures.
Their first step was to look at the literature to find the urine culture contamination rate benchmark. “We knew 45 percent wasn’t good, but we were shocked to learn through a CAP Q-Probes study that based on this study, at that rate we were in the less than 10th percentile of labs” (Bekeris LG, et al. Arch Pathol Lab Med. 2008;132[6]:913–917).
“We’re a laboratory that prides itself on quality, so this lit a fire in us because this is not where we want to be,” Peterson says. “And to get to even the median, we needed to get our culture contamination rate down to 15 percent.”
In June 2016, a mini refrigerator was installed in the microbiology laboratory setup area. “Low-hanging fruit. Easy to implement,” Peterson says. “Regardless of how long we expect setup to take of that specimen, it goes in the refrigerator.”

Peterson
In December 2016, nursing and physician leaders were brought into the conversation, and one month later laboratory staff had begun what Peterson calls a “tour of units.” In inpatient unit meetings, they discovered poor practices and a lack of understanding of the importance of the collection process, Peterson says, noting it was patient care technicians, not nurses, who in many cases were collecting the samples. “They didn’t understand there was a specific reason they needed to collect it in a sterile manner.”
In February 2017, she and colleagues introduced kits for clean-catch and foley-catheter collections. In each kit is an index card containing instructions and “a reminder of why this process is important to do appropriately,” she says. Also in the kit is a tube with preservative for culture testing, “so whether a urine culture is ordered or not, there is urine placed in the preservative tube. And once it hits the lab, it’s refrigerated immediately.”
For almost a year she and colleagues compiled data manually, and in January 2018, the overall urine culture contamination rate was 37.1 percent (106/286).
That month, she says, “we had a huge win.” A clinical intelligence dashboard was created for the project that would automatically pull monthly urine culture contamination rates for each inpatient unit and the emergency department. “We were able to then slice and dice that data in different ways to help us drive the project forward,” Peterson says.
By February, that meant monthly report cards sent to all units—with hospital administrator support—showing the prior month’s rate. “Every month a report card hit their inbox and it showed their unit’s contamination rate compared to all the other units in the hospital,” Peterson says. She and her laboratory colleagues were well aware of the variables and volume differences of the various units and how they affect a unit’s rate. Contamination rates of zero to 10 percent are reported in green, rates of 11 to 20 percent in yellow, and rates greater than 20 percent in red. The report cards were met with mixed reviews, she says. “But we all know what isn’t measured isn’t managed, and these leaders needed to see how their units were performing consistently.”
For some there was surprise about their rates, she says, and a few requests for a more limited distribution. “That report went out to everyone,” Peterson says, including hospital administration. “But once they discovered this isn’t punitive, and administration is not going to send them messages, they were on board and understood we needed to measure it.”
Though emergency department patients are not traditionally considered an inpatient population, the ED, with 24 beds at two locations—one ED attached to the hospital (plus seven overflow beds) and one freestanding ED—was included in the project because it accounted for many inpatient admissions and a large volume of urine testing orders. “Our ED partners were great to work with and extremely engaged,” Peterson says. ED leaders in May 2018 helped the laboratory team update and simplify patient collection instructions and standardize materials across all units. “We also simplified them to an eighth-grade reading level.”
Two years in, Peterson says, “We were starting to get discouraged.” The education and interventions failed to significantly decrease the urine culture contamination rate, which ranged from 37.1 to 39.9 percent between January and August 2018.
“At that point we asked ourselves, ‘What else can we do?’”
In August 2018, they took a closer look at the contaminated cultures to pinpoint the patient population source. A group of medical directors focused on the urinalysis reflex-to-culture orders. The criteria for reflex were a WBC greater than five/HPF, a positive leukocyte esterase, or a positive nitrate. They asked: “If we were to change these criteria to reflex only on a WBC greater than 10, what would happen to our data?” A retrospective study of any urine culture that would have reflexed using the old criteria but not with the new criteria revealed that more than 95 percent of the eliminated testing was unnecessary, Peterson says. “Within that subset there were contaminated cultures, no growth, or a nonpathogenic bacteria isolated.”
After standardizing the new reflex criteria, “we finally got that immediate dip in rates”: a urine culture contamination rate of 28.4 percent (58/204) in September 2018. Providers were still able to order a urine culture if clinically indicated (it wouldn’t reflex), but Avera McKennan’s urine culture contamination rate fell 10 percent “almost immediately,” she says.
By October, unit leaders proposed and implemented a new inpatient urine collection policy for using quick- or straight-catheter collections for patients who meet the standardized criteria, which led to an increase in those collections. By the end of 2018, the overall urine culture contamination rate, which began climbing above 31 percent after September 2018, had decreased to 28.6 percent (54/189).
“After our change in reflex criteria, we started talking more about unnecessary testing,” Peterson says. Jared Friedman, MD, clinical VP of emergency medicine for Avera Health, led a review of all emergency department order sets and in many cases eliminated urinalysis reflex-to-culture or urine culture orders embedded in the admission order sets. Physicians retained the ability to order a urine culture. “It just wasn’t embedded in their order set,” Peterson says.
By June 2020, the urine culture contamination rate was “finally headed in the right direction,” she says, reaching a low of 19.3 percent (22/114). “This was the culmination” of the steps taken to date.
In July 2020, Avera McKennan’s hospitalist team asked the laboratory to add Infectious Diseases Society of America guidelines-based queries to its urine culture orders to further address unnecessary urine culture testing.
“It’s just a pause,” Peterson says. If the person ordering can answer yes to any one of four queries, a urine culture is indicated.
They are as follows: Does the patient have dysuria, frequency, or urgency? Suprapubic pain/tenderness or costovertebral-angle tenderness? Unexplained fever of >100.4°F? Unexplained altered mental status changes in an elderly patient? If the answer to all of the queries is no, urine culture is not indicated. Providers still had the option to bypass the queries and order a culture.
“We were doing an average of 280 to 290 cultures a month” for the inpatient population at the outset of the project, and the number has dropped by more than 100 cultures a month, she says. “This decrease in testing was the result of the change in reflex criteria, the review of order sets, and the addition of the IDSA query.”
Over the course of the project, for the inpatient population and ED, urinalysis with reflex-to-culture orders decreased by more than 3,000 a year, Peterson says, and urine cultures performed decreased by more than 2,000 a year (Fig. 1).
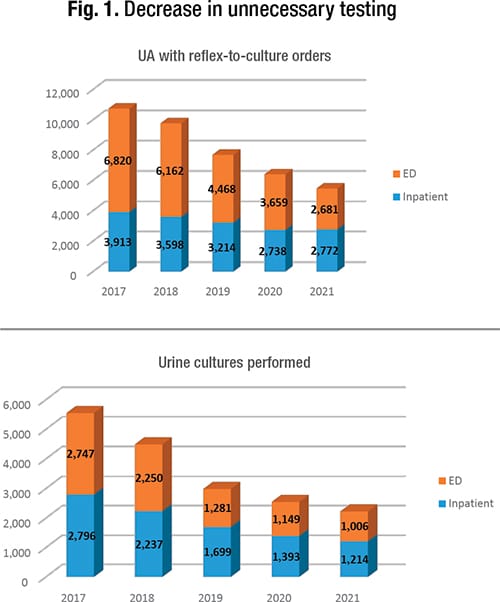
The hospital’s lowest combined inpatient and ED urine culture contamination rate of 16.9 percent was achieved in December 2020. Although the contamination rate never reached the 10 percent goal, the decline was significant, Peterson says, and had a positive impact on the patient population, physicians and nurses, and the laboratory. Nurses especially appreciated the decrease in unnecessary testing “because they don’t have to worry about collecting urine for a patient that’s not clinically indicated.” The new best practices were shared with other Avera Health hospitals, some of which have undertaken their own process improvement projects, Peterson says.
The laboratory team did work in the outpatient settings also, particularly in the obstetrics clinics. They standardized the collection materials and provided education for patients and staff, but no report cards are issued at this time. Improvements were seen, she says, and have been correlated with continual education for staff.
In 2021, during the pandemic, they took a step back and are still in a sustainment phase. The dashboard automatically captures inpatient data monthly and it’s monitored for unit numbers that stand out.
The estimated cost avoidance over three years was $3 million, Peterson says, and continues to be about $1 million annually compared with the starting point of the project. When estimating cost avoidance, they considered supplies, labor, and the impact of delays in results. “Urine cultures take 24 to 48 hours. You’re 24 to 48 hours behind the ball for that patient, which may result in an increased length of stay.”
There’s also an antibiotic stewardship component to consider if patients are treated unnecessarily with broad-spectrum antibiotics in the absence of a culture result to lead clinical treatment decisions.
“On the flip side, if you choose not to treat,” she says, “there could be a missed or delayed diagnosis for your patients, and the potential associated complications will likely be costly for the patient and the health care system.”
Another plus: a microbiology team that was pleased to be part of a project that required them to engage with other partners in the hospital, and greater visibility for the laboratory. “People learned who I was,” Peterson says, and the laboratory developed other partnerships “that we were able to carry into many other process improvement projects.”
Amy Carpenter Aquino is CAP TODAY senior editor. Peterson notes the contributions of Raed Sulaiman, MD, Cory Gunderson, Courtney Rosendahl, and the hospital and laboratory administrations.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
