Karen Lusky
May 2021—How to distinguish “reactive” and “nonreactive” benign lymphocytosis from malignant lymphocytosis, and between benign and malignant large granular lymphocytosis, is how Kyle Bradley, MD, of Emory University, opened his talk in a CAP20 virtual session last fall.
Dr. Bradley, associate professor of hematopathology and director of surgical pathology, co-presented with Olga Pozdnyakova, MD, PhD, on a morphology-based approach to hematopoietic neoplasms presenting with an abnormal WBC differential. (For coverage of Dr. Pozdnyakova’s talks on neutrophilia and monocytosis, see CAP TODAY, February and March 2021.)
“Some reactive lymphocytes can show very atypical morphologic features,” Dr. Bradley tells CAP TODAY, “and individual cells may understandably be worrisome for a lymphoid leukemia or lymphoma.” In these cases, it is important to review many lymphocytes on the smear to identify the broad spectrum of lymphocyte morphologies typical of a reactive lymphocytosis, he says.
Benign lymphocytosis with nonreactive morphologic features is often more of a mimic of malignant lymphocytosis, which is characterized by a monotonous population of lymphocytes. “The main feature for malignant lymphocytosis is that the lymphocyte population is atypical and monotonous in some way,” Dr. Bradley said.
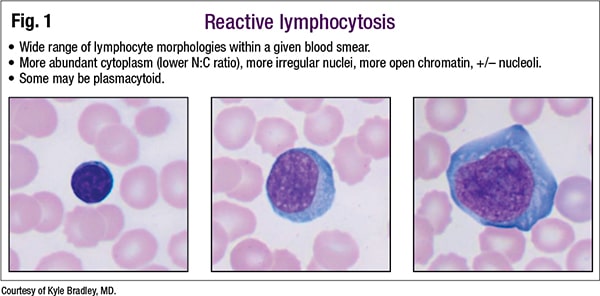
For reactive lymphocytosis, there is a wide range of lymphocyte morphologies within a given blood smear. “That’s the major feature you’re looking for,” he said, noting in Fig. 1 one small typical lymphocyte in the left image. In the center image is one that’s larger and more plasmacytoid appearing. The large lymphocyte on the right has more basophilic cytoplasm and some nucleoli. “This heterogeneity is a good feature for reactive,” he said. “More abundant cytoplasm on some of the cells is typical. Nuclei may be more irregular.”
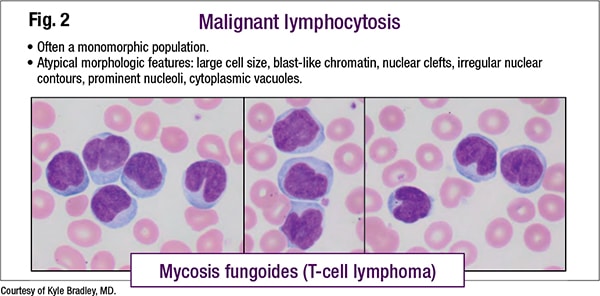
A typical malignant lymphocytosis is considerably more monomorphic (Fig. 2). “Some atypical features will be present. You may see normal lymphocytes in the background, so you get kind of a dimorphic population,” he said. Extensive blood involvement by mycosis fungoides, a type of T-cell lymphoma, can be seen in Fig. 2.
All of the lymphocytes are atypical, he said, and atypical in similar ways, with the chromatin slightly more dispersed than in a normal lymphocyte. There’s a little more abundant cytoplasm, and a lot of the lymphocytes have “interesting nuclear indentations, or grooves. So uniformity across the cells is the key feature that lets you know this is malignant.”
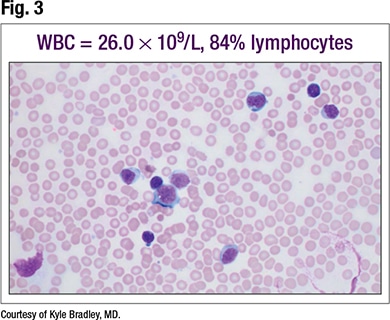
Dr. Bradley presented a case that he called the classic example of benign lymphocytosis with reactive morphology (Fig. 3). A six-year-old male had a white blood cell count of 26.0 × 109/L, 84 percent lymphocytes. “Even in this young age where they can have more of a lymphocytosis, this is still well above the reference range,” he said. (In adults, lymphocytosis is generally defined as an absolute count that exceeds 4.0 × 109/L.)
Every cell is lymphoid, but there is a variety of shapes and sizes. “Some of them are smaller cells. Some are distinctly larger and have more cytoplasm and more dispersed chromatin.” A smudge cell can be seen in Fig. 3 on the left, he said, and “a bit of a remainder of a smudge cell” on the right. Occasionally these can be seen in reactive lymphocytosis.
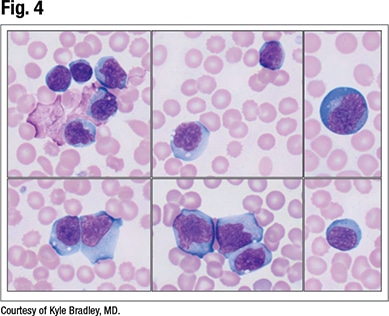
On higher power (Fig. 4), “sometimes these cases can look scary,” Dr. Bradley said. “Some of the cells can be quite frightening when you first put the smear down, but as you look around and start focusing in on the morphology, you can come to recognize that variety of shapes and sizes.” Some of the lymphocytes are small and look fairly normal. Some are large and have nucleoli and deeply basophilic cytoplasm. “And there’s a lot in between with more abundant cytoplasm.”
The clinician in this case suspected infectious mononucleosis and had already ordered EBV serology, which was indicative of an acute infection (positive IgM viral capsid antigen). The diagnosis was reactive lymphocytosis due to acute infectious mononucleosis.
 “You don’t need flow cytometry in these cases, but if you were to do flow cytometry, you should expect a predominance of cytotoxic T cells. And sometimes you can have decreased CD7 expression on T cells in these cases,” Dr. Bradley said.
“You don’t need flow cytometry in these cases, but if you were to do flow cytometry, you should expect a predominance of cytotoxic T cells. And sometimes you can have decreased CD7 expression on T cells in these cases,” Dr. Bradley said.
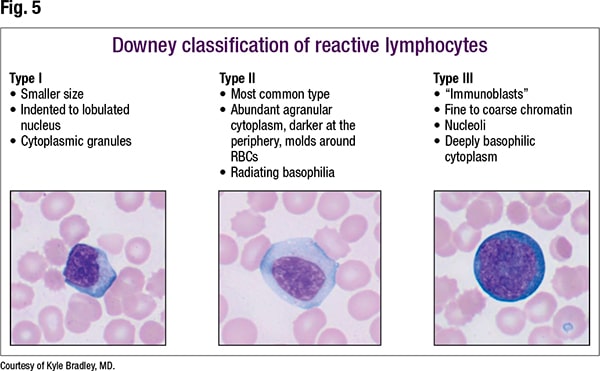
The Downey classification of reactive lymphocytes is not commonly used in current practice, he noted, but Downey identified, in 1923, three types of cells that defined the spectrum of reactive lymphocytes (Fig. 5). “And these are useful to recognize” when questioning if something is reactive. “I like to search around and find these different types. When I do, I feel much more confident and comfortable that, yes, this is indeed just reactive.”
Type I is less common than type II. “They’re smaller cells but still show atypical features. The nucleus usually has some degree of indentation, or maybe a little lobulation, and the cytoplasm is moderately abundant.” Cytoplasmic granules can be seen in type I.
Type II is the most common type of reactive lymphocyte and is characterized by a larger cell with abundant cytoplasm, he said. The nucleus that is generally round may be a bit irregular, and the chromatin is less condensed than in a normal lymphocyte. “You may get a slight, subtle hint of a nucleolus, but the nucleoli generally are not prominent. The cytoplasm has a characteristic feature—accentuated basophilia. Where it contacts the red blood cells, it often sort of molds around the red blood cells.” Radiating basophilia is a feature that he said is less discussed but fun to observe:
“It’s basically where the basophilia touches the red blood cells. It sort of radiates back to the nucleus.”
Type III cells, Dr. Bradley said, “are frankly immunoblasts, large angry-looking cells but with very coarse chromatin. A prominent central nucleolus is typical,” as is “deeply basophilic, royal blue cytoplasm.”
For lymphocytosis with reactive morphology, in the differential is not only infectious mononucleosis, the classic one and relatively common in practice, but also other viral infections (some cases of acute HIV and viral hepatitis; rarer would be adenovirus, HHV-6, rubella, roseola, mumps, chickenpox), especially acute cytomegalovirus, for which the morphology can appear identical to that of EBV. Parasitic infection (toxoplasmosis) and drug reactions are also in the differential. “The classic group [for drug reactions] would be anticonvulsants, especially phenytoin.”
 Flow cytometry usually is not needed in these cases, Dr. Bradley said, “because the morphology is classic, and then you correlate with the clinical history, and you can confidently sign these out as reactive.”
Flow cytometry usually is not needed in these cases, Dr. Bradley said, “because the morphology is classic, and then you correlate with the clinical history, and you can confidently sign these out as reactive.”
When is flow cytometry indicated? Dr. Bradley offers guidelines, not hard-and-fast rules. “Basically, anything that doesn’t fit right,” he said, referring to an atypical presentation—an older patient, for example, or clinical information inconsistent with a viral infection. Persistent lymphocytosis and non-classic lymphocyte morphology (less heterogeneous population, highly irregular or lobated nuclei) are other indications.
Dr. Bradley turned to large granular lymphocytosis, which he said “crosses the aisle between benign and malignant.” In Fig. 6 are three large granular lymphocytes (LGLs) in one field (an unusual quantity). “If the LGL count is not too high, you are kind of left wondering whether it is reactive or neoplastic. We can do ancillary studies,” Dr. Bradley said, “but a lot of times I’m signing these cases out as descriptive, and they need to correlate clinically” so a decision can be made on whether and how much to work it up.In reactive conditions, the absolute LGL count is often less than 2.0 × 109/L, he said. Post-bone marrow transplantation or post-chemotherapy are common etiologies, and some viral infections can increase LGLs. In his practice at an academic center where bone marrow transplants are performed, he sees modest increases in LGLs often. If there was a transplant, “we don’t work them up further,” and he reports it only in the microscopic description.
In contrast, neoplastic cases of LGLs usually are greater than or equal to 2.0 × 109/L. “Sometimes they can be less than that, but more than two should raise your suspicion that this may be neoplastic.” Most of these cases will be the cytotoxic T-cell type. NK-cell types also exist and can look similar morphologically.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
