Sherrie Rice
November 2022—Rapid next-generation sequencing in a community hospital setting, performed by histotechnologists and interpreted by anatomic pathologists, is possible and paying off, and it “makes the pathologist a much more meaningful part of the precision oncology team,” says Brandon Sheffield, MD, of the Department of Laboratory Medicine, William Osler Health System, Brampton/Etobicoke, Ontario.
“It has changed practice at our hospitals,” he says.

Dr. Sheffield
Dr. Sheffield, an anatomic and molecular pathologist, head of the Division of Advanced Diagnostics, and physician lead of research, says when pathologists can look at a case under a microscope, order NGS, and have the result the next day, “they gain a good appreciation for the relationship between what they’re seeing under the microscope and the results of the gene sequencing study.” He presented a CAP TODAY webinar, made possible by a special educational grant from Thermo Fisher Scientific, on how rapid NGS is supporting cancer care in the William Osler Health System, which includes three large community-based hospitals. (The full webinar is at captoday online.com.)
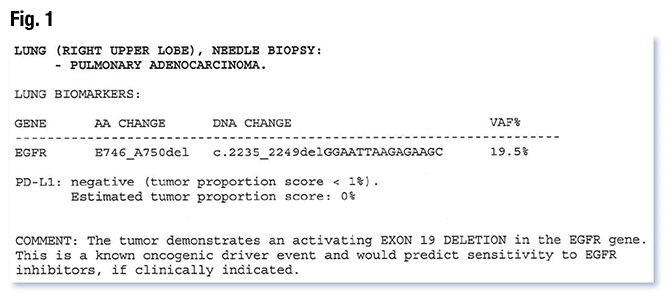
Dr. Sheffield illustrated how rapid NGS works using lung cancer as an example, which kills more Canadians than breast, colon, and pancreatic cancers combined—the number two, three, and four causes of cancer. And, like pathologists everywhere, “we’re responsible for a large number of actionable biomarkers that we need to test,” he said. In his practice, the biomarkers that must be reported to oncologists every time they treat a new lung cancer patient are PD-L1, EGFR, ALK, ROS1, BRAF, NTRK, HER2, NRG1, MET, RET, and KRAS.
“Colon cancer is not far behind,” he says of biomarker testing. “We have upwards of five different first-line systemic therapies that will be predicated on the biomarker results we provide to our oncologists.”
The mortality rate of untreated advanced lung NSCLC is four percent per week, he said. “I like to keep that front of mind when we’re working out the logistics of how our biomarkers are going to be delivered, because patients cannot get started on treatment without their biomarkers. And they’ll be looking at that high a mortality rate until we can issue those results.”
A molecular lab has 10 days to perform the biomarker tests and report results, according to consensus recommendations (Cheema PK, et al. Curr Oncol. 2020;27[6]:321–329). “Ten business days is two weeks in real time, and one of the issues we face in a community practice is that it’s exceedingly difficult for us sometimes to get the tissue to a molecular lab. The time we’re given in this guideline and others is three business days. However, it’s very difficult for many community labs to meet that,” Dr. Sheffield said.
“On the postanalytic side,” he added, “we’re told we need to get the information from a molecular lab into the hands of our oncologist in one day or less, and that again is difficult to achieve.”
He shared an example of how things worked before NGS was brought into the community hospital. A patient presented very ill to the hospital emergency department and was admitted to the oncology ward. It was a classic lung cancer presentation, he recalls, and the patient was too ill to be a candidate for chemotherapy but might have been able to be treated with targeted therapy. It took one week for the sample to be sent out for EGFR testing by next-generation sequencing. “That was what the normal process was like at the time.” Immunohistochemistry biomarker results, none of which was helpful, were available quickly. The patient subsequently died and a month later was found to be EGFR positive, L858R, by next-generation sequencing.“Sixty-two days from the time of diagnosis to receive that result. And that is the expected time frame for us when we’re sending out biomarker tests. Typically in a Canadian setting, a community hospital would send out results to an academic hospital within the same region, and that’s exactly what we expect—approximately two months turnaround time. All of our patients were faced with the same.”
IHC biomarker results were reported within a day. “So we wanted to explore to see if we could offer further biomarker testing. At the time, we could take things like ALK and ROS1 very far by IHC, but we were limited with markers like EGFR.”
In his practice, for breast cancer patients, the reports include not just a diagnosis of invasive ductal carcinoma, for example, but also the ER, PR, HER2, and IHC biomarker results. “To me, this is powerful, and when a patient is diagnosed in this way, the diagnosis is inextricable from the biomarker results. In a way, the patient is not being diagnosed with breast cancer; they’re diagnosed with hormone-receptor-positive breast cancer. And anytime a practitioner looks up that diagnosis, they’ll be forced to look at the same biomarker results, and this helps to steer the patient’s cancer journey in the right direction,” all of which is made possible by the IHC work performed onsite.
“Conversely, when we look at our molecular results, we tend to send them through a convoluted pathway, and this is why they take over a month.” Once a pathologist in the community makes the lung cancer diagnosis, the entire case would get shipped to an academic hospital, where it would then be accessioned and reviewed by another pathologist. That pathologist would have to assess the tissue for tumor content and cellularity, and possibly do IHC biomarkers like ALK or PD-L1. They would then ship that outside of their histology laboratory to a separate molecular laboratory for DNA and RNA extraction, library preparation, genome sequencing, and bioinformatic analysis. “And then an individual would sit down with all of these variants and write a report saying which of them are important and how these might impact treatments.”
The results typically would go back to the same anatomic pathologist at the academic hospital, who would sign off on the findings, possibly correlating them with IHC biomarkers. And then those results would be faxed to the original pathologist, who would then retype them into an electronic medical record and issue a report to their own oncologist. And that process in general took several weeks.
“So we set out to teach our IHC technologists to do next-generation sequencing. And to accomplish this, we used a highly automated gene sequencer”—Genexus Integrated Sequencer—“that was easy for them to use.” The technologists were taught how to de-paraffinize, digest the protein, and ultimately how to extract DNA and RNA and to quantitate and quality check it for sequencing. “Education and explanation” was all it took, Dr. Sheffield said, for them to make sure the specimens come through as needed.
“The technologist loading the instrument is the same technologist cutting the block and performing the diagnostic IHC. So they are our biggest ally in making sure the tumor cells make it from the block onto the gene sequencer.” If there is insufficient tumor content, “they’ll be the ones to spot it and help us out,” he said.
He and his colleagues validated the 50-gene Oncomine Precision Assay GX. To ensure the panel was fit for use in a clinical setting, validation was stringent and included small biopsies, cytology specimens, and surgical specimens, “the general milieu of what we experience in a pathology practice,” he said. “We found that this particular panel had a very high degree of concordance to reference methods for single nucleotide changes, for copy number alterations, as well as for RNA-based fusions.” Once the panel was validated, they combined the library preparation, sequencing, and bioinformatics into the automated sequencer and placed it directly within Osler’s IHC laboratory.
The anatomic pathologists were trained to report the variants, a new skill for many, Dr. Sheffield acknowledges. “And every pathologist is different,” with some needing more training than others, but “any pathologist can be trained in this,” he said. “Some of us will need more and some will need very little.” For those who need more, he recommends attending tumor boards and molecular courses at pathology conferences and talking to oncologists to learn how they use the results. Also helpful: having one person in the department with a bit more depth of knowledge. “Because that way, that person can do the more difficult cases, the more challenging cases, though the majority of results on a 50-gene panel are fairly straightforward.”
The typically lengthy turnaround time for NGS, in his view, hampers the ability of pathologists to gain a better understanding of NGS and how the findings might help them in their practice. “If you had a particularly challenging case and you send it out for NGS and don’t see the report for over a month, the question is now gone from your mind. You’ve moved on to new problems and issues. So it limits the ability.” Having both at the same time, on the other hand, “boosts the ability to learn and to better understand the interplay.”
Pathologists also find the NGS results can help them with their own pathology reports. “To better assess a questionable margin,” for example, Dr. Sheffield said. Or to determine the stage between two tumors that might be new primaries or metastases of one another. “They can even use [NGS results] for atypical cells that could be reactive or neoplastic. Getting a quick look at if there are any common mutations present in these can be a helpful diagnostic boost, and it didn’t take our pathologists very long to figure that out.”
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
