You and your coauthors write in the guide that a great debt is owed to Thinus Kruger, MB ChB, MD, of Tygerberg, South Africa, father of the modern morphologic evaluation known as Strict criteria. Can you tell us what his contribution to the benchtop guide was?
As a resident I was able to participate in an international research study and was introduced by email to Dr. Kruger, whose work has set the foundation for modern semen analysis. Dr. Kruger generously reviewed the images we provided of normal spermatozoa. Because the criteria he established—also known as Strict or Tygerberg criteria—are very specific regarding size, shape, and morphology of spermatozoa, most sperm on a stained slide are correctly classified as abnormal. In general, a typical semen analysis should not have greater than 25 percent normal sperm and, per WHO’s fifth edition, is only considered abnormal if less than four percent normal forms are present, approximately one in 20 sperm—much lower than the previous limit of 12 percent normal forms present. Different labs have set or chosen to follow different criteria, however, and our review of laboratory performance in QC for semen analysis shows a wide coefficient of variation in our Surveys of sperm morphology, often greater than 70 percent. This guide includes a short chapter on the different methodologies for reporting morphology, which explains some of this variation.
You also write that there is still wide variation between laboratories and observers despite the field of semen evaluation having evolved during the past three decades. Can you explain this variation and why accuracy is so important?
The variation between labs can be unsettling when initially reviewing the lab Survey results; how can one lab call 90 percent of the sperm normal when another lab reviewing the same specimen classifies only nine percent as normal? The reference guide devotes a chapter to the different classification systems used in reporting morphology and why that variation is present. We encourage labs to use the most recent guidelines from the WHO but do not compel them to do so. Regardless of the system used, it is important for labs to report which classification system they are using and the reference values the laboratory established.
How is the guide organized and why, and what might the reader want to know about the images?
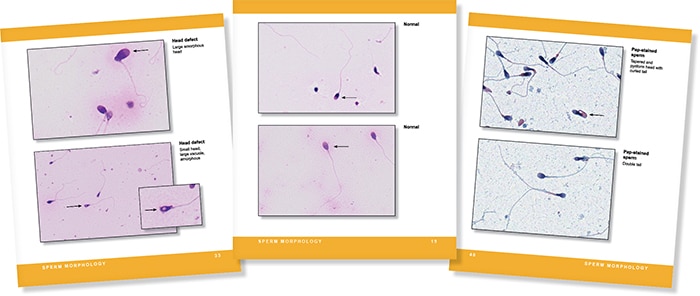
The guide is organized by the steps in the procedure with short sections for each reportable parameter in a typical semen analysis: liquefaction, volume, viscosity, pH, color, count, motility, viability, and morphology. Many stained images of normal and abnormal spermatozoa are included for reference. Feedback from reproductive laboratories we have surveyed included a strong interest to help in classifying non-semen cells present in semen, so many pictures of spermatids (precursors to spermatozoa), epithelial cells, and inflammatory cells are also included.
To order ($89), call the CAP at 800-323-4040 option 1 (item SABRG). If you are interested in writing a book for publication by CAP Press, contact Caryn Tursky at ctursky@cap.org.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
