Amy Carpenter Aquino
September 2022—Which biomarker for heart failure should be used—BNP or NT-proBNP—and does it matter?
That’s the question Christopher W. Farnsworth, PhD, assistant professor of pathology and immunology, Division of Laboratory and Genomic Medicine, Washington University School of Medicine in St. Louis, set out to answer in his “hot topic” talk (one of a trio) at the AACC meeting in July.
The two natriuretic peptide methods have an overall poor correlation, end-stage renal disease affects NT-proBNP more than it does BNP, and one of the therapies used to treat heart failure affects BNP but not NT-proBNP, Dr. Farnsworth explained. Still, they’re relatively comparable for diagnosing heart failure, he said, though they can’t be interchanged.
When his laboratory switched from using BNP to NT-proBNP for patients with suspected heart failure, he and his colleagues used both assays for three months, in 2017, on every physician-ordered BNP, Dr. Farnsworth tells CAP TODAY. Both sets of results were recorded in the electronic health record so providers could rebaseline their heart failure patients who had been monitored serially with BNP but who now would get an NT-proBNP result. It was “also to help rebaseline the providers,” says Dr. Farnsworth, who is also medical director of clinical chemistry and the core laboratory at Barnes-Jewish Hospital.
Dr. Farnsworth and colleagues found low concordance between two commercially available BNP and NT-proBNP assays for ruling in and ruling out heart failure in acute and nonacute settings (Farnsworth CW, et al. Clin Biochem. 2018;59:50–55). Patients with eGFR <60 mL/min/1.73m2 had decreased concordance and increased NT-proBNP-to-BNP ratios relative to patients with eGFR >60 mL/min/1.73m2. “This suggests that different cutoffs may be required in patients with CKD [chronic kidney disease],” he and his coauthors wrote.
While the Pearson correlation for all samples—ED and nonED—was good at 0.71, the linear regression r2 was “not particularly good at 0.51,” he said. And “we are most concerned with results that are at or near critical decision points.”
“When patients present with heart failure,” Dr. Farnsworth said, “the cardiomyocytes in the heart recognize the stretch on the heart because there’s fluid overload.” In response, they start to synthesize and produce pro-BNP, which is cleaved at the 76th amino acid.
This process makes two separate molecules: “NT-proBNP, which is made up of the first 76 amino acids and is biologically inactive” and “in a one-to-one molar ratio with BNP.” BNP, a biologically active hormone, will have downstream natriuretic effects to clear sodium and water, he said. “It does a great job of trying to relieve a lot of those pressures on the heart and the system to try to reduce that cardiac stretch.”

Dr. Farnsworth
A prospective study of 1,586 patients seen in the emergency department found that “the ideal cutoff for ruling out patients [with congestive heart failure] was a BNP of 100 picograms per mL, which has a sensitivity of 90 percent and a specificity of 76 percent,” Dr. Farnsworth said, calling BNP an “effective biomarker when thinking about ruling patients out with a high negative predictive value” (Maisel AS, et al. N Engl J Med. 2002;347[3]:161–167).
In a meta-analysis published in 2006, Januzzi, et al., looked at the performance of NT-proBNP for diagnosing congestive HF and “basically showed the same thing,” Dr. Farnsworth said: “Those who have heart failure had much higher concentrations of NT-proBNP” (Januzzi JL, et al. Eur Heart J. 2006;27[3]:330–337).
“The caveat here is that NT-proBNP increases with age,” he said. Januzzi, et al., had three ROC curves: for patients under age 50, for patients 50 to 74, and for patients over 75. They established age-specific cutoffs, “and when they did that, they found that across all ages they had a sensitivity of exactly 90 percent—same as BNP—and a similar specificity [84 percent],” Dr. Farnsworth said. Which raises the question: which biomarker to use and does it matter?
“The guidelines are remarkably neutral, probably as neutral as a guideline can be,” Dr. Farnsworth said of the AHA/ACC/HFSA Guideline for the Management of Heart Failure, which says the values of BNP and NT-proBNP can be used in the patient care setting, “but not which one you should use.” But the guideline writers later added: “as long as their respective values and cutpoints are not used interchangeably.”
“Slightly more helpful,” Dr. Farnsworth said of the addition, “but what does that mean?”—particularly for hospital systems in which patients are transferred between hospitals where different methods may be used for detection of natriuretic peptides.
It’s not just BNP and NT-proBNP that don’t correlate particularly well, Dr. Farnsworth said, referring to a 2014 study (unpublished) in which Siemens compared its BNP assay to three other BNP assays. Results correlated well until measurements reached the 100 pg/mL cutoff, above which the differences in the four assay results were relatively significant, he said.In another study, one looking at the differences in recovery among BNP assays, the authors showed “recovery across various systems is variable” though “not incredibly dramatic,” Dr. Farnsworth said (Luckenbill KN, et al. Clin Chem. 2008;54[3]:619–621). “But in some cases you’re looking at a 15 percent higher recovery relative to others and relative to the exact same concentration of another BNP.”
One of the reasons, he said, has to do with the antibodies of detection. “These are generally two-step immunoassays, so they’re using two separate antibodies.” Some manufacturers target the N-terminus, some the C-terminus, and others the ring epitope, he said, “and this molecule, because it’s a hormone, has a relatively short half-life and starts to degrade as it’s circulating. So if your assay happens to detect the N-terminus amino acids, and that BNP’s been circulating for a while, you’re not necessarily going to be able to detect that molecule if you’re trying to capture it in this region, as opposed to a manufacturer that’s detecting in the ring epitope.” The results will differ slightly, he said, even across BNP assays.
NT-proBNP assays are far more standardized with regard to the antibodies used, Dr. Farnsworth said. “They’re licensed to one company, and several companies use the same antibodies. All the companies that have them are targeting the same region. Nevertheless, they still get very different recoveries.”
Harmonization is one reason. “There’s not really good reference material. But there’s also interesting biochemistry happening here, some of it due to translational modifications,” he said.
Some of the inability to detect NT-proBNP and why it may vary a little depending on the platform has to do with glycosylation of the peptide itself, Dr. Farnsworth said, citing another study published in 2008 (Seferian KR, et al. Clin Chem. 2008;54[5]:866–873).
NT-proBNP becomes spontaneously glycosylated, he said, and Seferian, et al., demonstrated this by making monoclonal antibodies (MAbs) against various regions of the NT-proBNP peptides. They concluded: “The central part of endogenous NT-proBNP is glycosylated, making it almost ‘invisible’ for the antibodies specific to the mid-fragment of the molecule. Thus sandwich assays using even one antibody (poly- or monoclonal) specific to the central part of the molecule could underestimate the real concentration of endogenous NT-proBNP.” They added, “MAbs specific to the N- and C-terminal parts of NT-proBNP (epitopes 13–24 and 63–76) are the best candidates to be used in an assay for optimal NT-proBNP immunodetection.”
“All commercially available assays actually target this region with their antibodies,” Dr. Farnsworth said. “That tells us, particularly in chronic heart failure patients, they’re more likely to have glycosylations and to get some amount of moderate recovery.” Thus, by some of these assays, “you’ll get variable performance.”
Other factors known to affect natriuretic peptide concentration, he said, are obesity (decreases production), chronic kidney disease (increases NPs), and glycosylation with renal failure (decreased).
Dr. Farnsworth presented the case of a 72-year-old male with diabetes, shortness of breath, blood pressure of 154/98, and severe edema around the ankles, seen first at a small outside hospital where his BNP was measured at 90 pg/mL. When transferred to Barnes-Jewish Hospital, his NT-proBNP concentration was 1,100 pg/mL. Does this patient have heart failure? Dr. Farnsworth asked.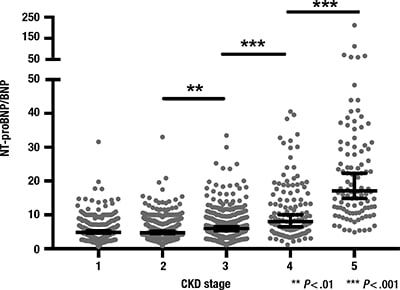
Fig. 1. Increased NT-proBNP relative to BNP in patients with chronic kidney disease
The accepted cutoffs for BNP and NT-proBNP measurements in the acute setting were derived from the Maisel, et al., and Januzzi, et al., studies. For patients under age 75, heart failure is ruled out with a BNP of <100 pg/mL or an NT-proBNP of <300 pg/mL, “and that is a very strong negative predictive value,” Dr. Farnsworth said. The only HF rule-out difference in the assay cutoffs is for patients age 75 or older, for whom the NT-proBNP cutoff is <450 pg/mL (BNP<100).
He described the gray zone of accepted cutoffs where heart failure is possible. For BNP at all ages, it’s 100–500 pg/mL. For NT-proBNP: <50 years, 300–450 pg/mL; 50–74, 300–900 pg/mL; 75 and over, 450–1,800 pg/mL.
In the rule-in category, more differences are seen in the accepted cutoffs for NT-proBNP measurements, Dr. Farnsworth said. The BNP cutoff is >500 pg/mL for patients of all ages. For NT-proBNP: <50 years, >450 pg/mL; 50–74, >900 pg/mL; 75 and over, >1,800 pg/mL.
In the case of the 72-year-old patient with a BNP of 90 pg/mL and an NT-proBNP of 1,100 pg/mL, by one assay (BNP) he does not have heart failure and by NT-proBNP he does. The way to approach this case is to think about concordance, Dr. Farnsworth said—how well these assays agree using those cutoffs, which he and his coauthors addressed in their study published in 2018 of 2,729 patient samples obtained in the ED and non-ED settings.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
