Charna Albert
September 2022—A single high-sensitivity cardiac troponin T measurement below the limit of quantitation of 6 ng/L is a safe and rapid method to identify a substantial number of patients at low risk for acute myocardial injury and infarction, say the authors of a recently published study (Sandoval Y, et al. Circulation. 2022;145[23]:1708–1719).
Allan S. Jaffe, MD, senior author of the study and professor of both cardiology and laboratory medicine and pathology at Mayo Clinic in Rochester, Minn., said Mayo Clinic developed a two-hour algorithm and did not initially embrace the single-sample rule-out. “That’s not because there wasn’t good data about the single-sample rule-out with cardiac troponin T. There actually was,” Dr. Jaffe said in a session at this year’s AACC annual meeting. In fact, he and his coauthors write in the study, extensive data from outside the U.S. support the single-sample rule-out when hs-cTnT concentrations are below the limit of detection of 5 ng/L. However, the FDA does not permit reporting values down to that level. The lowest reportable level is less than 6 ng/L, and Dr. Jaffe notes that the data for using that value are much less robust.

Dr. Jaffe
“One of the reasons this works—and this is important and not often talked about—is not just because there is the time that allows for the egress of troponin to get to the circulation, but because if you look at all the risk factors that lead to underlying cardiovascular and atherosclerotic disease, they almost all cause modest increases in troponin values, albeit within the normal range.” So a very low troponin value, he said, not only can exclude myocardial infarction in most instances but also is an indication that the patient doesn’t have a large number of risk factors for atherosclerotic disease.
“The reason we went to a two-hour protocol as well as not using the first sample rule-out has to do with the analytics of the assay,” he said. An imprecision profile from one of the original studies of the Roche high-sensitivity cardiac troponin T assay shows that in distinguishing between a change of 3 ng/L and a change of 5 ng/L, “which is a distinction advocated for use with the one-hour protocol, you’re going to have some misses and some overlaps,” he said, and the same is likely to happen in distinguishing between a value of less than 5 ng/L (limit of detection) and less than or equal to 6 ng/L (limit of quantitation) (Saenger AK, et al. Clin Chim Acta. 2011;412[9–10]:748–754).
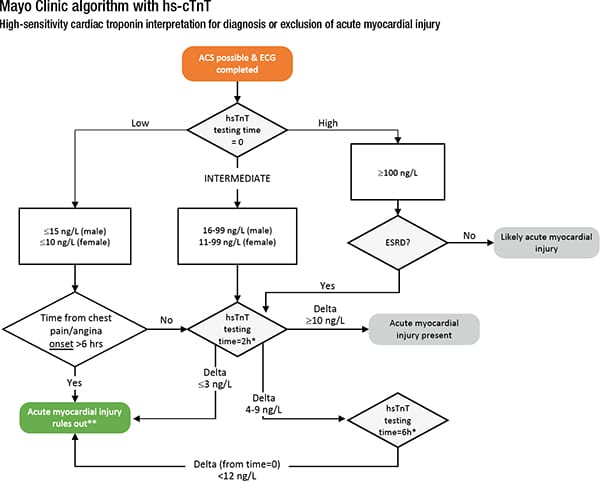
*If chest pain began >12 hours ago, a negative delta does not rule out recent myocardial injury. **Consider unstable angina may require additional evaluation. This document is intended to help guide decision-making for evaluation of ACS. This does not supersede clinical judgment.
This problem related to imprecision is not unique to high-sensitivity cardiac troponin T. Dr. Jaffe and others found that the value of Abbott’s high-sensitivity cardiac troponin I assay can change when repeated on the same sample over a period of time, which calls into question the clinical applicability of the European Society of Cardiology 0/1-hour algorithm to rule out and rule in myocardial infarction. They took 50 random heparin plasma samples (stored at room temperature) and measured for high-sensitivity cardiac troponin I at three times, all within 3.5 hours of the first measurement. Their goal was to evaluate the analytical variation of results in the same samples when measured multiple times over a period and to determine the misclassification rate associated with the European Society of Cardiology 0/1-hour algorithm and the two-hour algorithm due to short-term analytical variation (Kavsak P, et al. Clin Chem. 2017;63[6]:1163–1165).
Almost half (24) of the samples had values that might be applied at the rule-in or rule-out level—either very low (﹤7 ng/L) or within 10 ng/L of the rule-in value (52 ng/L). Seven of the samples would have resulted in a different categorization, depending on the sample reported. This was the case in particular with values that might be used at one hour (2 ng/L versus 6 ng/L), where six of the 18 patients would have switched diagnostic categories from rule-out to observe, Dr. Jaffe said. “So a third of patients would have shifted diagnostic categories just by repeating the same sample, and it’s a reflection of the imprecision of the assays, particularly at lower values.”
In addition, during Mayo Clinic’s analytic validation, substantial differences for hs-cTnT were found among the various instruments (Donato LJ, et al. Am J Clin Pathol. 2021;156[6]:1121–1129). “In addition, we had a flyer rate of 3.4 percent using a change rate of 3 ng/L, and a flyer rate of one percent using a change rate of 10 ng/L,” he said. “These were the reasons why we were concerned that if we used the single-sample rule-out of 6 ng/L, or a delta trying to distinguish in the one-hour algorithm between three and five, we were for sure going to misclassify substantial numbers of patients.”
“That’s why we went to a two-hour protocol and did not embrace single-sample rule-out.”
This was the reality for high-sensitivity cardiac troponin T, but for many assays “using single values substantially above the limit of detection—and therefore reportable—allowed one to rule out substantial numbers of patients.” But for troponin T, the value validated in Europe for single-sample rule-out was less than 5 ng/L, a concentration threshold that isn’t available for clinical use in the U.S. And in Europe, Dr. Jaffe and his coauthors write in Circulation, troponin testing isn’t used as broadly as it is in the U.S., so European data from more selected chest pain populations may not be as informative for U.S. practice. “The FDA only allows reporting for troponin T to a value of less than 6 ng/L, because of the imprecision of values below that number. So one had to ask the question, could a value of less than six be equally good?”
In their recent study published in Circulation, the goal of Dr. Jaffe and his coauthors was, first, to determine whether a single high-sensitivity cardiac troponin T (Roche Elecsys Troponin T Gen 5 Stat) below the limit of quantitation of 6 ng/L is a safe strategy to identify patients at low risk for myocardial injury. Second, to evaluate the use of this approach in identifying patients at low risk for acute myocardial infarction, they examined the combined use of a nonischemic ECG with a hs-cTnT of less than 6 ng/L in an adjudicated cohort.For the first goal, they drew on data from the CV Data Mart Biomarker cohort, a multicenter (22 sites), observational biomarker study involving consecutive adult patients who presented to a Mayo Clinic emergency department and in whom at least one hs-cTnT measurement was obtained within 12 hours of presentation from the date of site-specific hs-cTnT implementation until December 2020. A total of 85,610 patients were evaluated (mean age 63 and 50 percent women). Of the total, 24,646 (29 percent) had a baseline hs-cTnT of less than 6 ng/L. Of these, 49 (0.2 percent) had acute myocardial infarction diagnoses based on ICD-10 codes and 19 (0.1 percent) deaths occurred during the index presentation.
Sex-specific analyses demonstrated that women were more likely than men to have a baseline hs-cTnT of less than 6 ng/L (38 percent versus 20 percent of men, P﹤0.0001). And compared with men with hs-cTnT less than 6 ng/L, women with hs-cTnT less than 6 ng/L were older and more likely to have comorbidities, except for previous myocardial infarction and coronary artery disease, which were more frequent in men.
Acute myocardial injury (any subsequent hs-cTnT increase above the sex-specific 99th percentile) occurred in 146 (1.2 percent) of the 11,962 patients with a baseline hs-cTnT of less than 6 ng/L with serial measurements, resulting in a negative predictive value of 98.8 percent (95 percent CI, 98.6–99.0) and sensitivity of 99.6 percent (95 percent CI, 99.5–99.6). Among the patients who developed acute myocardial injury, maximum hs-cTnT concentrations were 20 (14–43) ng/L.
“The negative predictive value of less than six for men was very high,” Dr. Jaffe said. “For women, on the other hand, there was an occasional signal that suggested it was less than perfect, particularly in older women, usually with cardiovascular comorbidities.” Of the 146 false-negative cases, 117 were women and 29 were men. Among those with a baseline hs-cTnT of less than 6 ng/L, 0.7 percent of men (29/4,264) and 1.5 percent of women (117/7,698) developed acute myocardial injury. Adjudication of the 146 cases demonstrated that 76 percent (111) were attributable to isolated nonischemic acute myocardial injury. The remaining 35 cases (25 women and 10 men) were classified as acute myocardial infarction.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
