Valerie Neff Newitt
November 2022—Burnout among Canadian pathologists is prevalent, pain related for some, and workload driven for many. “There needs to be more of us,” says Julia Keith, MD, associate professor in the Department of Laboratory Medicine and Pathobiology at the University of Toronto and neuropathologist and director of wellness, Department of Laboratory Medicine and Molecular Diagnostics, Sunnybrook Health Sciences Center, Toronto.
Dr. Keith is the author of a study published online Aug. 8 in the Archives of Pathology & Laboratory Medicine, titled “The Burnout in Canadian Pathology Initiative” (doi:10.5858/arpa.2021-0200-OA). Four hundred twenty-seven pathologists completed a survey across all 10 Canadian provinces, for a response rate of 50 percent of all Canadian Association of Pathologists members and 27 percent of all pathologists practicing within Canada. Most respondents (363) had completed the survey pre-pandemic, by March 2020. Sixty-four responded mid-COVID-19, in October 2020. There was no significant difference in the prevalence of burnout between the pre- and mid-pandemic cohorts.
Burnout was defined using the Maslach Burnout Inventory—Human Services Survey for Medical Personnel (MBI-HSS) and characterized by three domains: emotional exhaustion, depersonalization (feeling cynical or having a callous approach toward others), and a low sense of personal accomplishment (feeling ineffective in one’s work).
“The headline is the prevalence,” Dr. Keith says of the survey’s findings. “Fifty-eight percent of Canadian pathologists are burned out. And we know that physician burnout has negative implications for physicians themselves and for the quality of care they provide. So that’s a big deal.”
“Physician well-being, and pathologist well-being in particular, is a topic that warrants a great deal more scholarship,” she says.
In the study, workload was found to be the top source of job-related stress, followed by ineffective leadership and stressful relationships (Fig. 1). It’s no surprise that workload came out on top, Dr. Keith says. “Workload is widely known as the major driver of physician burnout. So what can be done about it?” In response to an open-ended question about what pathology departments are doing to mitigate burnout, “some respondents described the process of workload assessment and subsequent attempts to distribute cases consistently and equitably as effective burnout mitigation strategies,” Dr. Keith says. “But the vast majority of workload-related departmental initiatives [reported by respondents to be effective] involved successful advocacy for more pathologist positions, more locum tenens. So I suspect our community needs to grow.”
Many workforce-related decisions are driven “by metrics, by evidence,” she adds. “So I’m hopeful that data from studies like this that demonstrate pathologist burnout prevalence can be useful to those who are advocating at various levels for more pathologist positions.”
A logical next step, in her view, could be to investigate the link between pathologist burnout and the quality of care pathologists provide. “Given the rigorous way that quality metrics are documented in laboratory medicine, our field is well positioned to study the relationship between physician burnout and medical error—patient safety—better than what has been done previously.”
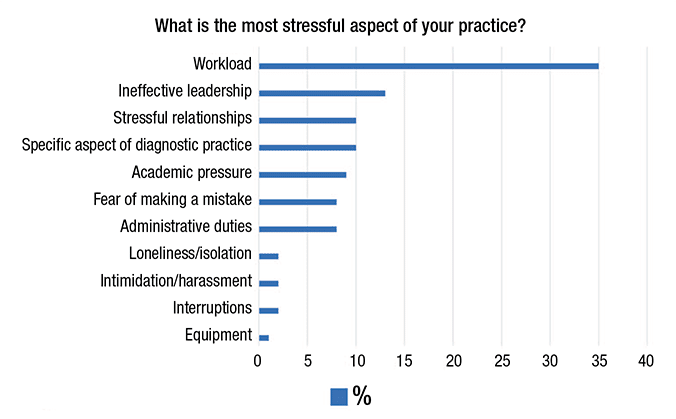
Fig. 1. Top sources of job stress for Canadian pathologists shown as percentage of total responses mapping to each of 11 identified themes. From Keith J. Arch Pathol Lab Med. Published online Aug. 8, 2022. doi:10.5858/arpa.2021-0200-OA.
Another way to confront the physician burnout problem: build a business case for addressing burnout because of the associated physician turnover, reduced work effort, and early retirement. “These phenomena are financially costly,” Dr. Keith says.
An important finding of the study, she says, is the “relatively untapped opportunity for improvement” in practice flexibility. “The greater the amount of flexibility a given pathologist felt their department allows significantly correlated with lower scores on all domains of burnout.” Digital pathology and other such innovations in the field, she says, “have the capacity to allow for much more flexibility in when and where and how we do our work, and I am looking forward to seeing whether they have an impact in reducing pathologist burnout.” For pathology leaders, she adds, “I would encourage them to try to creatively foster flexibility in their own departments.”
Dr. Julia Keith: “The greater the amount of flexibility a given pathologist felt their department allows significantly correlated with lower scores on all domains of burnout.” [Photo by: Kevin Van Paassen/Sunnybrook]
“The fundamental building block for wellness infrastructure is to appoint somebody as your physician or pathologist wellness lead, and then protect some of their time so they can do the job well,” she says. They need time to pursue training in physician well-being, such as the Stanford Physician Well-Being Director Course, to conduct needs assessments, and to implement wellness initiatives that are informed by local need, Dr. Keith says. “And involve your wellness lead in your leadership team.” There are sources of guidance not just for individuals, she says, but also for institutions that want to address burnout at a system level. They include, for example, programs of the National Academy of Medicine and the AMA. Hospitals that choose to participate in the AMA program, titled Joy in Medicine Health System Recognition Program, are awarded various levels of recognition based on their level of commitment to reducing burnout. “One of the takeaways for me when I read about these programs,” Dr. Keith says, “is how important it is for organizations to be able to demonstrate that they’re making operational decisions that take physician well-being into consideration, because in the absence of that, one runs the risk of whatever wellness infrastructure has been built as being viewed as a token gesture.”
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
