Charna Albert
January 2023—Guidelines for the diagnosis of von Willebrand disease, published in 2021, have raised questions about which von Willebrand factor activity assay laboratories should use. Each has its strengths and weaknesses, and the FDA has cleared or approved some, but not all, of the newer automated assays. In addition, not all the assays or guidelines use the same activity-to-antigen ratio cutoff to discriminate type 1 from type 2 von Willebrand disease, making it difficult to compare accuracy.
“That just begins the challenge,” said Marian Rollins-Raval, MD, MPH, associate professor of pathology at the University of New Mexico and medical director, TriCore Special Coagulation Laboratory, speaking in a CAP22 session about the five major types of von Willebrand factor (VWF) activity assays. Then, too, more clinical studies evaluating the newer assays and comparing them with the original ristocetin cofactor assays are needed, said co-presenter Neil Harris, MD, clinical professor of pathology, immunology, and laboratory medicine at the University of Florida. Drs. Rollins-Raval and Harris are members of the CAP Hemostasis and Thrombosis Committee.
When assessing a patient with a bleeding tendency for von Willebrand disease (VWD), Dr. Harris said, start with a CBC, “because it could be a thrombocytopenia.” Prothrombin time and partial prothrombin time should be measured because PT is not prolonged in VWD. “You’ll want to look at fibrinogen and possibly the thrombin time as well,” he said. If results of all are normal or there’s an isolated prolonged PTT, “you want to do the initial VWF screening assays,” which include VWF antigen, VWF activity, and factor VIII activity. If one or more of these tests are abnormal, the patient should be referred for selected specialized VWD studies, including von Willebrand multimeric analysis (James PD, et al. Blood Adv. 2021;5[1]:280–300; Nichols WL, et al. Haemophilia. 2008;14[2]:171–232).
The first VWF activity assay was the ristocetin cofactor assay. “The original tests were done by optical aggregometry and were really lab-developed tests using fixed reagent platelets,” Dr. Harris said. These assays had poor precision and a high coefficient of variation, he said, leading to low intraassay and interlaboratory reproducibility. “But the ristocetin cofactor assay became the gold standard simply because it was the first assay.” It has since been automated on some coagulation analyzers, he said, and those assays typically use a commercially available reagent containing lyophilized donor platelets and ristocetin. “If you have the correct coagulation analyzer, you can do it with a turbidimetric analysis and you can measure the platelet agglutination and compare it with calibrators and controls,” he said. The automated assay, which is FDA cleared, has better precision than the aggregometry assay, but the limit of detection is not substantially improved.
The overall algorithm for diagnosis of VWD laid out in the 2021 American Society of Hematology, International Society on Thrombosis and Haemostasis, National Hemophilia Foundation, and World Federation of Hemophilia guidelines begins with the VWF antigen, platelet-dependent VWF activity, and factor VIII activity (James PD, et al. Blood Adv. 2021;5[1]:280–300) (Fig. 1). If VWF levels are greater than 50 IU/dL, VWD can be ruled out, Dr. Harris said. “If it’s less than 30 percent, you’ve diagnosed von Willebrand disease, but the next step is the activity-to-antigen ratio. We typically do a platelet-dependent VWF activity—which up until now was the ristocetin cofactor activity—divided by the von Willebrand factor antigen.” (The algorithm says VWF level 30 to 50 for simplicity; this refers to VWF levels of 0.30 to 0.50 IU/mL, with the caveat that the lower limit of the normal range as determined by the local laboratory should be used if it is less than 0.50 IU/mL.)
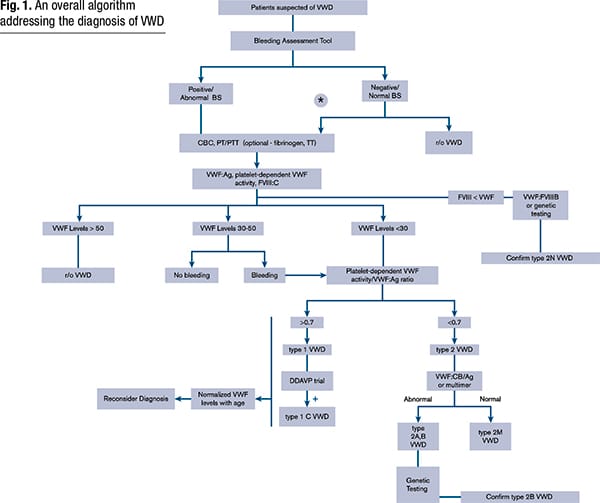
VWF levels refer to VWF antigen (VWF:Ag) and/or platelet-dependent VWF activity. The algorithm says VWF level 30 to 50 for simplicity; this refers to VWF levels of 0.30 to 0.50 IU/ml, with the caveat that the lower limit of the normal range as determined by the local laboratory should be used if it is <0.50 IU/ml. *Men and children, referred to a hematologist and/or first-degree relative affected with VWD. BS, bleeding score; CBC, complete blood count; DDAVP, desmopressin; FVIII, factor FVIII; FVlll:C, FVIII coagulant activity; PT, prothrombin time; PTT, partial thromboplastin time; r/o, rule out; TT, thrombin time; VWF:CB/Ag, ratio of VWF collagen binding to antigen; VWF:FVIIIB, VWF FVIII binding.
Reprinted from Blood Advances, vol 5(1), James P, Connell N, Ameer B, et al. ASH ISTH NHF WFH 2021 guidelines on the diagnosis of von Willebrand disease, pages 280–300, Copyright 2021, with permission from Elsevier.
Per this new algorithm, a ratio of more than 0.7 classifies the more common type 1 VWD, caused by a partial quantitative deficiency of VWF. A ratio of less than 0.7 classifies the patient with type 2 disease, which encompasses the qualitative VWF defects and where “von Willebrand factor may be present in normal amounts, it may be reduced in some cases, but it’s lost some function,” Dr. Harris said. These are subclassified, most commonly, as types 2A, 2B, 2M, and 2N.

Dr. Harris
Those with intermediate levels of VWF activity (0.30–.50 IU/mL) are classified as “low VWF” if they have no bleeding, he said. “But if they have bleeding they would be put in the von Willebrand disease category.”
Type 2N, Dr. Harris said, is the functional variant in which “von Willebrand factor does everything in its normal capacity, except it lacks the ability to bind to factor VIII.” For patients with suspected type 2N in need of additional testing, the 2021 guidelines suggest using either VWF:factor VIII binding studies or targeted genetic testing for type 2N variants.
One of the problems with the ristocetin cofactor assay, Dr. Harris said, is the D1472H polymorphism, a common VWF ristocetin-binding polymorphism that reduces the apparent activity. When it’s present, “the ristocetin cofactor will give a low reading even though there are no clinical consequences,” he said. “It’s an in vitro effect, not an in vivo effect, and can lead to the overdiagnosis of von Willebrand disease.” The polymorphism (present in the A1 domain) is found in 63 percent of Blacks and 17 percent of the white population.
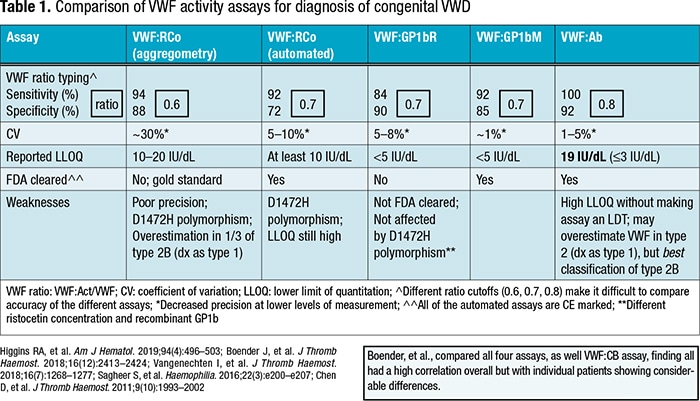
The guidelines suggest glycoprotein (GP) 1bM or GP1bR, newer automated assays that measure platelet-binding activity of VWF, over the automated or nonautomated ristocetin cofactor assay. “They call it a suggestion rather than a recommendation because the evidence wasn’t very certain,” Dr. Harris said. At the time the guidelines were published neither of these assays was FDA cleared, but one GP1bM assay received de novo FDA approval in 2022.
The GP1bR assay works as follows: In the presence of ristocetin, patient VWF binds recombinant wild-type GP1b attached by monoclonal antibodies to GP1b onto latex or magnetic beads. “If you add ristocetin and patient von Willebrand factor, the beads will agglutinate, and this can be monitored by an immunoturbidimetric or chemiluminescent assay.” The assay is not FDA cleared, though some laboratories have developed their own versions of both the GP1bR and GP1bM assays, he said.
“The GP1bM is a variation on the same idea,” Dr. Harris said. “You have a latex bead that’s coated with GP1b by virtue of a bridging antibody, except that the GP1b is a gain-of-function mutant which binds spontaneously to von Willebrand factor, to the A1 domain. So it’s exactly the same as the previous assay, except it doesn’t require ristocetin.” (The “R” in GP1bR stands for ristocetin, he noted, and the “M” in GP1bM stands for mutant.)
The VWF antibody assay is FDA cleared and gaining in popularity, Dr. Harris said. “When somebody first described this assay to me I said, ‘This can’t possibly work.’ But it does work,” he said. Without ristocetin, latex beads coated with monoclonal antibodies against the VWF A1 domain agglutinate with the addition of patient VWF. “I thought it wouldn’t work because I thought it would only pick up mutations in the A1 domain. But it was explained to me—and this was borne out by evidence—it also picks up defects in multimerization.” The antibody assay, which is available on some automated platforms, “is a great screen to discriminate patients with and without von Willebrand disease.”
With the antibody assay, additional VWF activity tests are likely to be needed for subclassification. “You certainly need the multimers and you may need collagen binding as well,” he said. The VWF antibody assay has similar sensitivity and specificity to the ristocetin cofactor assay, though it has comparatively increased precision and a decreased coefficient of variation at lower levels. It typically uses a VWF:Ab/VWF:Ag ratio of less than 0.7 to discriminate types 1 and 2, “though people have used higher ratios,” he said. “In our lab we run this assay. If the activity comes out low or less than 55 percent, we will reflex to the ristocetin cofactor assay.”
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
