Karen Lusky
March 2022—Most thyroid cancer cases are straightforward, but a small percentage are not. In a CAP21 molecular oncology tumor board session, Justin Bishop, MD, and Saad Khan, MD, spotlighted one of the latter.
Dr. Bishop, the Jane B. and Edwin P. Jenevein, MD, distinguished chair in pathology and professor and chief of anatomic pathology, UT Southwestern, and Dr. Khan, assistant professor of medicine (oncology) at Stanford, took a look at two unusual cases of head and neck cancer, the first of which was reported in the February issue (captodayonline.com). This month: medullary thyroid cancer.
Because medullary thyroid cancer can be aggressive, Dr. Bishop said he would advise pathologists to have a very low threshold for excluding it on any thyroid cancer with an unusual appearance. “I have definitely seen cases where it was misdiagnosed on FNA, where it was called Hurthle cell neoplasm,” he said. While diagnosing medullary thyroid cancer is often straightforward, he said, it’s not always straightforward.
The case he and Dr. Khan reported on is that of a 49-year-old male who presented with a 2 × 3-cm neck mass centered around a right nodule. It was painless but enlarging over time; no change in voice or swallowing was noted. There was no family history of thyroid problems or cancer or hereditary syndromes. The patient was referred to an endocrine surgeon who found in his workup a right thyroid lobe mass with associated lymphadenopathy. He was diagnosed with medullary thyroid carcinoma based on fine-needle aspiration. Serum CEA and calcitonin were markedly elevated. Total thyroidectomy and neck dissection were performed.
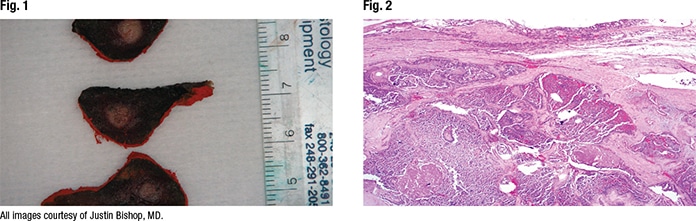
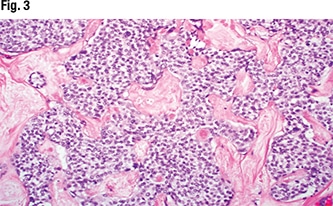
In Fig. 1 is the gross examination, “where we have this kind of ill-defined tan-white nodule centered in the thyroid lobe,” Dr. Bishop said. At low power, it’s an infiltrative, solid-looking tumor showing areas of fibrosis and hemorrhage (Fig. 2). “At high power, we have this kind of monotonous-appearing clear-cell tumor embedded in hyalinized stroma” (Fig. 3).
“Even more prominent stroma that is very likely to be amyloid” can be seen in Fig. 4, Dr. Bishop said, as can cells that are uniform, “almost plasmacytoid-looking in areas, with kind of amphophilic to clear cytoplasm, resembling a carcinoid tumor or other low-grade neuroendocrine tumor in another site. In this anatomic location,” he said, “neuroendocrine carcinomas are known as medullary carcinoma.”
In Fig. 5 are lymph nodes “filled with this same-looking tumor, which makes sense given the lymphadenopathy that was seen clinically.”
The characteristic histology made TTF-1 unnecessary in this case, but if validation were needed to confirm a case of medullary carcinoma, TTF-1 could be performed, Dr. Bishop noted (Fig. 6). That TTF-1 is positive in medullary carcinoma surprises some pathologists, he said. “Thyroglobulin, of course, will be negative in medullary carcinoma in contrast to follicular-derived thyroid cancers” (Fig. 7).
Calcitonin, the marker typically used to diagnose medullary carcinoma, is not always positive in medullary, Dr. Bishop cautioned. He also orders CEA routinely for medullary carcinomas, and usually both are positive, “but at least one of them should be positive to call something a medullary carcinoma,” he said. A neuroendocrine tumor will be positive for synaptophysin and chromogranin as well. The pathology in this case, he said, “was fairly straightforward, as most medullary carcinomas will be.”
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
