In the week before the CAP21 session in which he and Dr. Bishop presented, Dr. Khan saw three divergent cases of medullary thyroid cancer. “One is an almost infectious malignant medullary thyroid cancer,” where the tumor is growing extremely rapidly. “It’s creating a superior vena cava syndrome,” and has spread to the large vessels of the mediastinum. Therapy was to be started immediately. “And it makes absolutely no sense,” Dr. Khan said.
A second case that he said makes no sense is one in which the patient was diagnosed 15 years earlier with a neuroendocrine tumor in the head and neck region that remained stable and for which surgery was performed five years later, with a diagnosis of medullary thyroid cancer. “And it was quiescent for the next 10 years—some residual disease, elevated CEA and calcitonin, then nothing.” The patient now has fulminant disease and is being treated with radiation.

In the third case, the patient’s CEA and calcitonin were rising. A metastatic medullary thyroid cancer that had been removed surgically had returned, and the patient complained of gastrointestinal dysfunction, “a typical finding of these medullary thyroid cancers that are more advanced.” Dr. Khan prepared to start the patient on targeted therapy, “and suddenly his numbers started plummeting for no reason,” and his diarrhea began to resolve. “These are the real head-scratchers where even though these are all confirmed, perfect diagnoses of medullary thyroid cancer, there is something funny going on about all of it. We are not able to capture the full understanding of why some patients have really aggressive malignant-behaving medullary thyroid cancers and others do not.”
Dr. Khan said the case of the 49-year-old patient presented in the CAP21 session followed the more aggressive, rapidly recurrent path more typical of medullary thyroid cancer. Post-surgery, the patient’s calcitonin and CEA were in the normal range, but after nine months, they started to rise to above three times the upper limit of normal. CT imaging of the chest showed more than 10 new subcentimeter nodules that could not be biopsied. The patient was asymptomatic. Pulmonary nodules were more numerous six months later but couldn’t be biopsied easily.

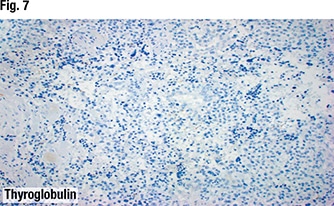
The patient then reported an enlarged left testicle. Urologic consultation and ultrasound and other imaging suggested a solid mass, but it was one that could not be classified further noninvasively. The patient underwent orchiectomy, which found metastatic medullary thyroid cancer that metastasized to the testicle. “This disease can metastasize to odd areas, and it can confuse people in that it almost disguises itself in where it goes, how it proceeds, and in these episodes where, for a duration of time, it is rapidly progressing and then suddenly it stops and fools you into a false sense of security,” Dr. Khan said.
Post-orchiectomy, the calcitonin and CEA decreased to 20 percent of peak but were still elevated. Molecular testing performed on the orchiectomy specimen finds the RET M918T mutation. Dr. Khan said he orders next-generation sequencing on every metastatic medullary thyroid cancer patient. “It comes back positive more often than not,” though he can’t provide statistics at this time, he said, because germline RET abnormalities have to be taken into account as well as somatic, as does the patient population. “But it is often a shock to me when RET comes back as negative,” he added.
“It’s critical for us,” he said of the mutation and what it means for oncologists and patients, thanks to two drugs the FDA approved in 2020: selpercatinib (Eli Lilly) for lung and thyroid cancers with RET gene mutations or fusions, and pralsetinib (Blueprint Medicines) for RET-altered thyroid cancers. “Until 2020, the best drugs we had had significant toxicities,” Dr. Khan said.
The 49-year-old patient with the RET M918T mutation had numerous symptoms attributed to the metastatic medullary thyroid cancer and was started on a clinical trial four years after he initially saw Dr. Khan for his original diagnosis of metastatic medullary thyroid cancer. “He had a fantastic, rapid response within about a week, and visible disease started to resolve,” an indicator that in the “weird” cases of medullary thyroid cancer, Dr. Khan said, “finding a RET mutation can make all the difference in the world in the patient’s daily life, quality of life, and likely length of life as well.” This is why, he said, molecular testing is being performed—or should be—on all patients with metastatic medullary thyroid cancer.
Karen Lusky is a writer in Brentwood, Tenn.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
