The tool’s sepsis score tracker recalculates the patient’s sepsis score every 15 minutes. “It’s dynamic,” he said. “It’s not a one-time score.”
Epic’s performance results showed a positive predictive value of 16 percent with a threshold set at four percent, and a positive predictive value of 50 percent if the prediction threshold is set at 40 percent, according to an Epic report. “The negative predictive value was very similar, irrespective of where you are,” he said: 93 percent with a prediction threshold of four percent and 97 percent with a threshold of 40 percent. “I’m not surprised by this. This is trying to optimize the model in such a way where we are not missing anybody and no one is falling through the cracks.”
But the specificity needs improvement, Dr. Isbell said, noting that it’s unclear at this point if treatment of patients classified as likely to have sepsis is harmful or contraindicated. “It is an active area of research for us at Saint Louis University Hospital and the sepsis committee I sit on.”
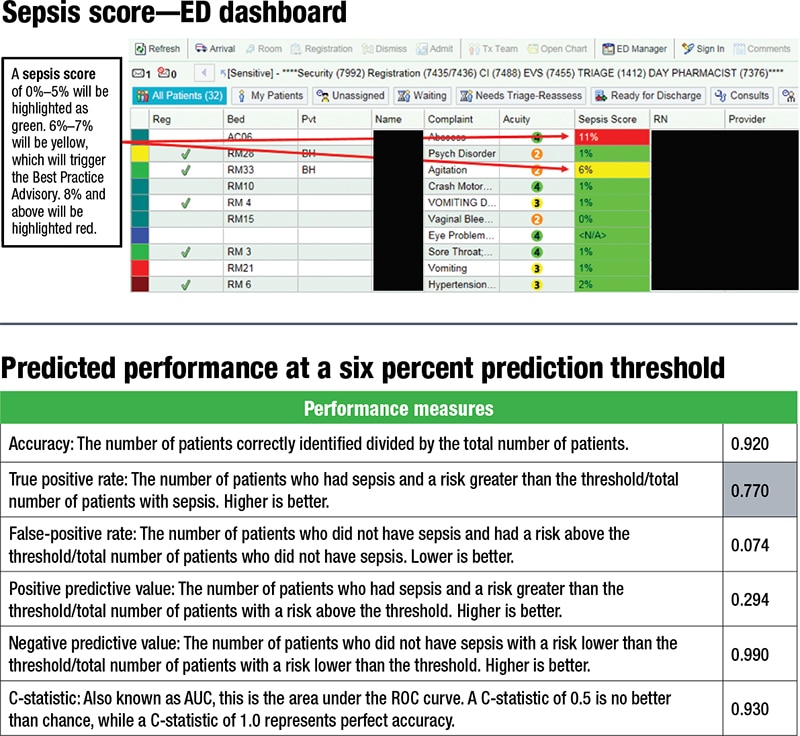
A tool can be used to “play around with the threshold,” Dr. Isbell said. If he and colleagues set theirs at six percent, they’re expecting to see a positive predictive value similar to what was seen at 30 percent, and a negative predictive value at 99 percent. “This tool allows for some level of customization depending on desired outcomes and patient populations.” (See “Predicted performance at a six percent prediction threshold.”) “What we’re trying to do now is collect the actual data and see how in real life does this stack up to what our predictive performance would be.”
He and colleagues are monitoring the sepsis alert firing frequency by location and the response rate—the number of alerts responded to within 30 minutes. “We’re probably at 50 to 60 percent, so we have more work to do in terms of people acting on that order set. A teaching hospital complicates that because new people come in and move around.”
They’re also monitoring the SEP-1 outliers. “Are we adhering to the model, are we ordering blood culture, are we giving them fluids? Are we doing all these things like we’re supposed to?
“To summarize, I think predictive analytics is a tool that can help identify patients likely to become septic,” Dr. Isbell said, adding that the tool needs fine-tuning. “Our main goal is to be able to predict with a high degree of sensitivity and specificity those likely to develop sepsis, treat them, and prevent them from developing or advancing to septic shock.”
Amy Carpenter Aquino is CAP TODAY senior editor. Amanda Thompson, RN, BSN, patient safety and quality coordinator and chair of the SSM Health SLU Hospital sepsis committee, provided some of the data and other information Dr. Isbell presented at the AACC meeting. Dr. Isbell presented in the same session as David Ford, PhD; see story.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
