In Fig. 15 is an example of CLL in which a monotonous population and the characteristic coarse “soccer ball” chromatin are seen, Dr. Wojcik notes. “They are a little larger than regular mature lymphocytes, but it would be difficult to evaluate in fluids. A lot of lymphocytes—make sure it goes for flow.”
Cell blocks can present challenges, too, Dr. Jiang said, noting that she often sees rare, atypical cells on the ThinPrep or cytospin. “And with cell block, you may not see a really distinct population of big cannonballs,” she said. “You may just have one or two single cells that are atypical. If you’re using immunos in that context, be really cautious about making the definitive diagnosis of malignancy when dealing with single cells.” Some cases surprise, she said. “You do the GATA3 or the ER and everything lights up. But often it’s rare single cells that maybe have a little TTF or a little GATA3 in the cell block.”
“That’s why we still have the indeterminate diagnosis,” Dr. Wojcik said. “This is for cases where we try to work it out, and despite our efforts, we cannot make the diagnosis straight. However, we cannot ignore them.” If the patient reaccumulated fluid quickly, that’s a red flag to look at this much more seriously, she said.
Sometimes, Dr. Jiang said, it’s simply a case of the cytopathologist catching the tumor early on, when there is little tumor burden. “A couple of weeks later, they recollect, and then it becomes much more obvious. We’re catching tumors at different points in their biology.”
“What if we’re left with something that looks mesothelial and stains mesothelial and then looks malignant?” Dr. Jiang asked.“We make a diagnosis of mesothelioma,” Dr. Wojcik replied, noting it’s the subject of controversy, especially in cytology. Malignant mesothelioma is a serious diagnosis, but there is an opportunity for management and patients have a chance for an extended survival if diagnosed early, she said.
All of the characteristic features of mesothelial cells will be seen in mesothelioma: grasping, clasping, cannibalism, prominent nucleoli, multinucleation, and the others. One way to differentiate: There will be more of those features and all will be larger, Dr. Wojcik said (Fig. 16).
“When you see huge macronucleoli, think potentially about mesothelioma,” she said (Fig. 17). Near perfect symmetry and vacuolization can also be seen.
Nuclear atypia is where the controversy lies, she said (Fig. 18). It’s not classically striking, “especially when you see the uniformity of cells.”
Another clue: small, orangeophilic squamous-like cells (Fig. 19). “This is where we are going to zoom and think, Is this a squamous cell carcinoma? But they don’t have enough atypia for it to be a squamous cell carcinoma.” The diagnosis can’t be made based on these cells, she noted, “but when you see them, think, Could this be a case of malignant mesothelioma?”
Fig. 20 is “mesothelioma in cytology in real life,” she said, noting they were the most abnormal case she could find, confirmed by IHC as mesothelial. In cases like that, she said, “there’s no way we can make the diagnosis on cytology even if we are aware that the concomitant surgical specimen was diagnosed as mesothelioma.”
How to make the diagnosis? First, establish the mesothelial phenotype. (Only the epitheloid type of mesothelioma, or a mixed type with a significant epithelial component, will shed the cells that can be evaluated, she noted.) The next step is to establish malignancy by FISH (deletion of the 9p21 region/loss of p16 [CDKN2A]). Other markers: BRCA1-associated protein 1 (BAP1) mutations (loss) and methylthioadenosine phosphorylase (MTAP) 9p21.3-related protein (loss). “It’s very important to have an internal control,” she added.
Thus, cytology specimens can be used but the diagnosis shouldn’t be made on morphology alone. Malignant mesothelioma in situ “is real,” she said, noting the consensus of experts. Dr. Wojcik’s approach to malignant mesothelioma on cytology is what she calls “another triple test” (Fig. 21). In a case with a characteristic morphology and an encasing mass on CT, for example, “I don’t need cytology. I know it’s malignant mesothelioma,” she said, adding that it can be confirmed by loss of BAP1. For legal purposes, she said, if there is certainty based on morphology, clinical radiographic presentation, and markers, it’s better for all to make the definitive diagnosis. Use of “consistent with” is likely to raise questions.





If the clinical presentation suggests malignant mesothelioma and there is a characteristic morphology but the markers are inconclusive, the diagnosis is “malignant cells most consistent with malignant mesothelioma.” If something doesn’t make sense, she said, “we have to leave ourselves room.”





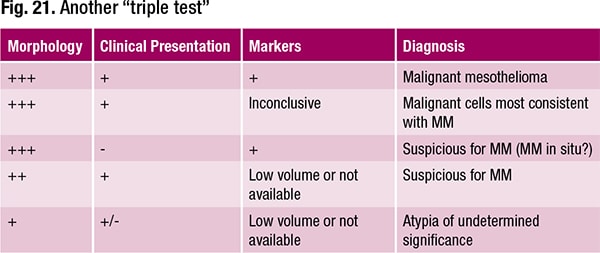
If the clinical exam turns up nothing but the markers are consistent with malignant mesothelioma along with a positive control of benign mesothelial cells, “you cannot ignore it,” she said. “You can’t let it go. You have to tell clinicians they have to find something. This is potentially mesothelioma in situ.”
If there’s a mass but an insufficient or unavailable specimen for additional studies to confirm malignancy, it’s atypia of undetermined significance and there must be follow-up.
“Whatever you do, avoid extremes,” she advises. “All the pieces in your puzzle—morphology, clinical/radiographic findings, and, most importantly, adjuvant tests—have to line up to make a diagnosis of malignant mesothelioma in cytology.”
Sherrie Rice is editor of CAP TODAY.
 CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
CAP TODAY Pathology/Laboratory Medicine/Laboratory Management
